×
Il semble que vous utilisiez une version obsolète de internet explorer. Internet explorer n'est plus supporté par Microsoft depuis fin 2015. Nous vous invitons à utiliser un navigateur plus récent tel que Firefox, Google Chrome ou Microsoft Edge.

Devenez membre d'Incathlab et bénéficiez d'un accès complet !
Vous devez être membre pour accéder aux vidéos Incathlab sans limitation. Inscrivez vous gratuitement en moins d'une minute et accédez à tous les services Incathlab ! Vous avez aussi la possibilité de vous connecter directement avec votre compte facebook ou twitter en cliquant sur login en haut à droite du site.
Inscription Connexion
Inscription Connexion
This didactic procedure concerns a 77 years old Women with diabetes , HBP, Dyslipidemia , presenting infra abdominal and lower limbs resting pain and bilateral trophic ulcers , due to distal abdominal aortic calcified occlusion . After multimodality assessment of lesions, she has undergone percutaneous abdominal aortic angioplasty and stenting with good final result.
Step-by-step procedure: How to deal with symptomatic Abdominal Aortic calcified occlusion
Educational objectives
- How to manage patients with lower limbs resting pain and abdominal Aortic occlusion
- Multimodality assessment of aortic occlusion before the intervention
- How to plan access, procedural steps, and selection of devices
- How to preserve renal artery and mesenteric artery during distal abdominal aortic occlusion
- How to prepare for stenting by Intra-Vascular Lithotripsy
1) Access sites:
- Brachial access : 6 French access using micro puncture system (COOK)
- Femoral access: 7 French access using micro puncture system (COOK)
- Heparin administration
2) Abdominal Aorta catheterization:
- Continuous flushing of the guiding catheter while introducing guidewire
- Advance softly an 6 Fr JR 4 guiding catheter to the descending aorta over a J 3 0.035’’ GUIDEWIRE
- Advance the 0.035” Guidewire towards the top of the aorta occlusion
- Advancing 70 cm 6F Braided SHEATH (Cook Flexor ® )
3) Crossing Aortic occlusion :
- With the support of the 6F catheter and a stiff angulated guidewire “0.018” Halberd wire Asahi®.
4) Pre-dilatation of the lesion with 6 x 80 mm Sterling balloon BSC
5) IVL Dilatation of the lesion with SHOCKWAVE balloon 8 mm x6cm , inflated to 4 ATM
6) Femoral retrograde recrossing of the aortic lesion using 0035’’ guidewire Advantage Terumo ® and BERENSTEIN 6F Catheter MERIT MEDICAL ®
7) Switching to Femoral introducer Sheath 12F , 45 cm Cook Flexor ®
8) Stenting
- Select the precise spot of stent deployment , in order to preserve collaterals . Control by brachial introducer
- Deployment of 14 x 49 mm Stent BeGraft Peripheral BENTLEY ® inflated to 5 ATM (two times)
- Control post stenting result , renal artery and mesenteric artery preserved
- Verify if there is any dissection or Rupture
9) Final angiographic control: ( 2 views Frontal & Lateral)
10) Vascular femoral closure with an 8 Fr Angio-Seal™
11) Medical adjunctive treatments
- Pre-procedural: Heparin , propofol and midazolam.
- Post procedural : double therapy: Aspirin 75mg o.d. + Clopidogrel 75mg o.d for one month
- After one month : Stop Clopidogrel and continue Aspirin 75mg
Bibliography
Date du tournage : 30/03/2023
Dernière mise à jour : 11/07/2023
Dernière mise à jour : 11/07/2023
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Partager
Participer à la discussion
Suggestions
TEVAR of the thoracic aneurysm with short neck below left common carotid artery using C TAG with act...
Case of the month: March 2022
Partager
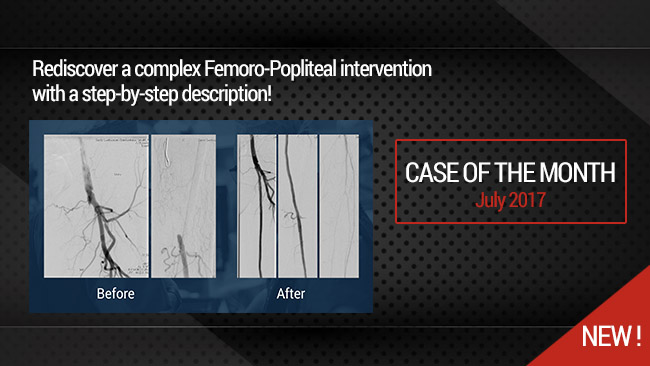
Long Femoral Occlusion (35 cm) - Subintimal crossing and extra long stenting
Case of the month: July 2017
Partager
Live case #5 from Swiss CTO Summit 2019 - Dr Avran & Dr Faurie
Case of the month: February 2020
Partager
Simultaneous treatment of two coronary artery bifurcations in three vessels disease patient
Dedicated coronary bifurcation stents - Case of the month: May 2018
Partager
Diffuse coronary multivessels disease. Complex PCI treatment
Case of the Month: February 2018
Partager






Eli P. Thank you!
Muhanad A. Very nice one