×
Il semble que vous utilisiez une version obsolète de internet explorer. Internet explorer n'est plus supporté par Microsoft depuis fin 2015. Nous vous invitons à utiliser un navigateur plus récent tel que Firefox, Google Chrome ou Microsoft Edge.
My Player placeholder

Devenez membre d'Incathlab et bénéficiez d'un accès complet !
Vous devez être membre pour accéder aux vidéos Incathlab sans limitation. Inscrivez vous gratuitement en moins d'une minute et accédez à tous les services Incathlab ! Vous avez aussi la possibilité de vous connecter directement avec votre compte facebook ou twitter en cliquant sur login en haut à droite du site.
Inscription Connexion
Inscription Connexion
18338 vues
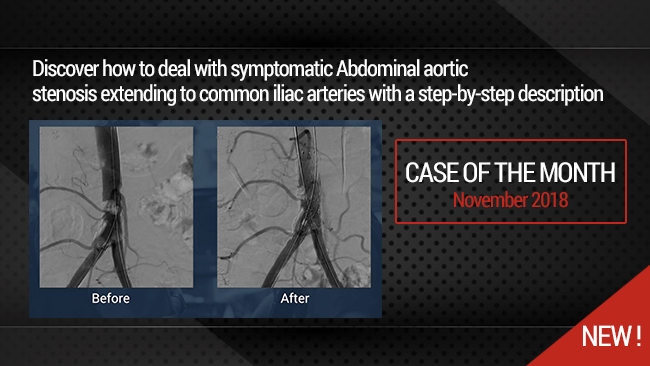
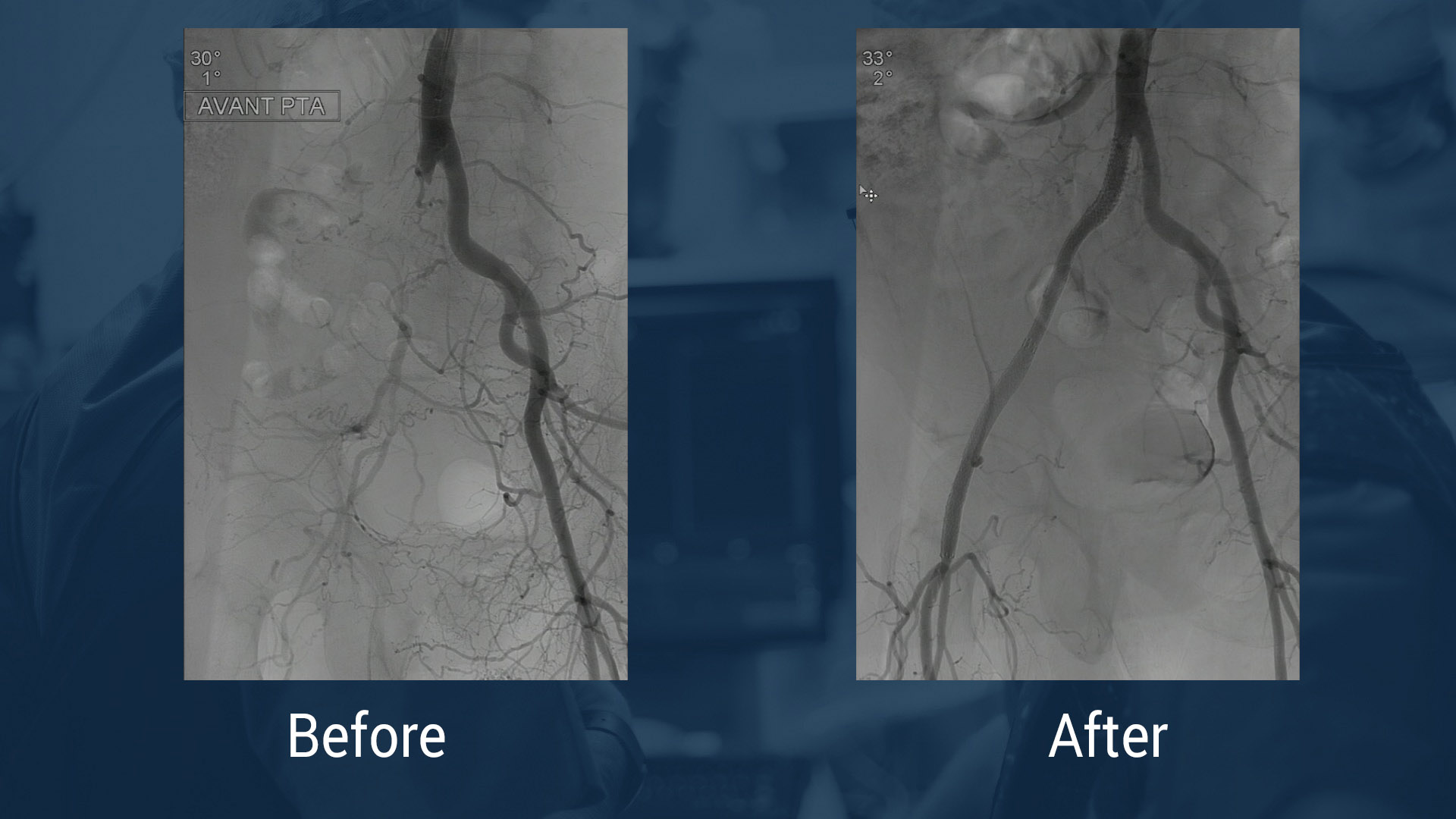
This didactic procedure concerns a young heavy smoker lady with bilateral lower limb severe claudication, presenting distal abdominal aortic calcified stenosis extending to bilateral common iliac arteries. After multimodality assessment of lesions, she has undergone percutaneous abdominal aortic & bilateral iliac angioplasty and stenting with good final result.
Educational objectives
- How to manage patients with intermittent claudication and Aorto-iliac stenosis.
- Multimodality assessment of aorto-iliac stenosis before the intervention.
- How to plan access, procedural steps, and selection of devices.
- How to preserve inferior mesenteric artery during distal abdominal aortic stenting.
Step-by-Step description
- Selection of femoral site: Left Femoral artery access with 7F 23cm introducer.
- Right Femoral artery access under Roadmap guidance (6F 23cm introducer).
- Crossing both iliac arteries & Aortic stenosis with 0.035" Advantage guidewire (Terumo).
- Aortic predilatation with a 10x40mm at 8ATM.
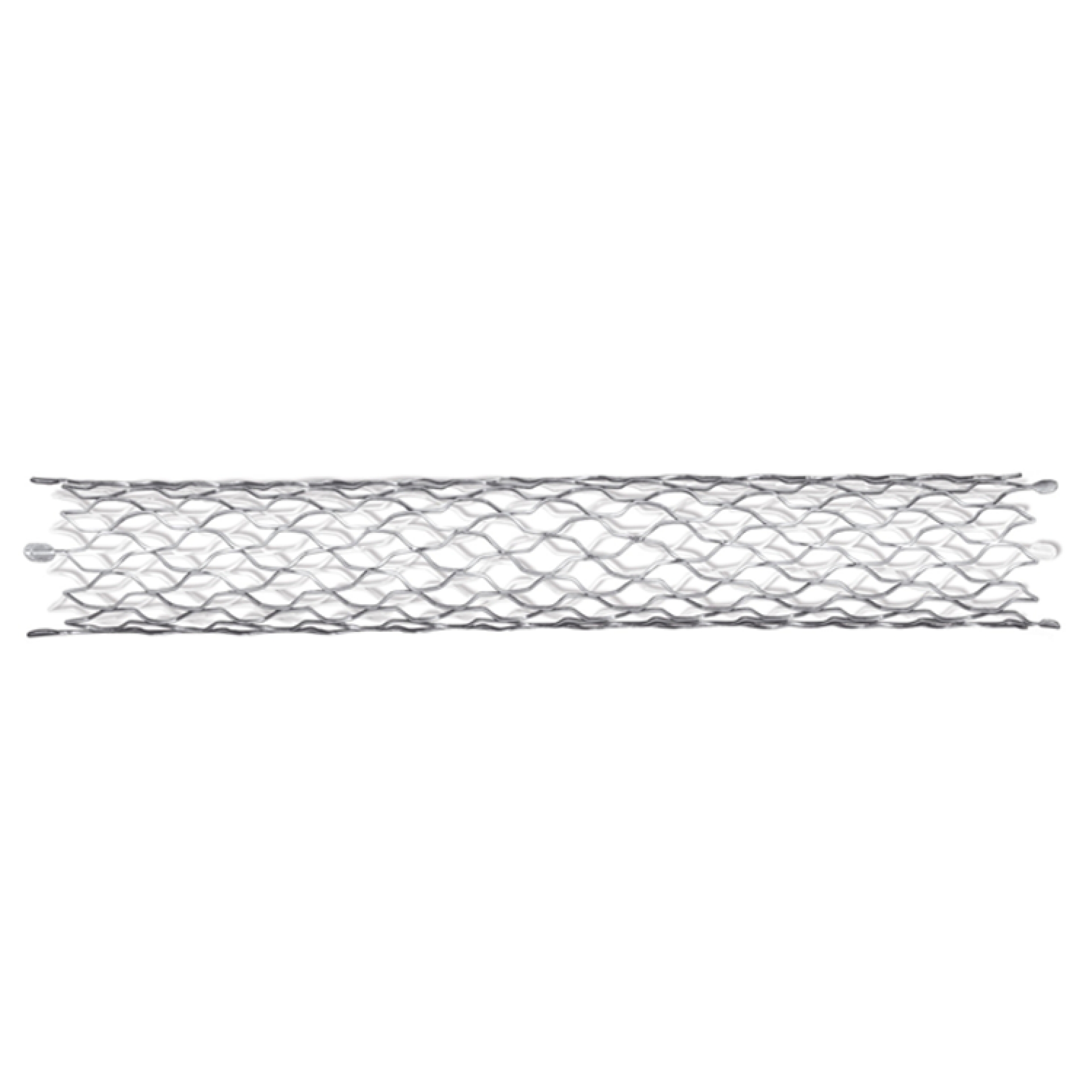
- Autoexpandable Stent implantation in the distal Aorta under Roadmap guidance: OPTIMED 12X40mm over the 7F Sheath.
- Recross the aortic stent with the right 0.035" guidewire.
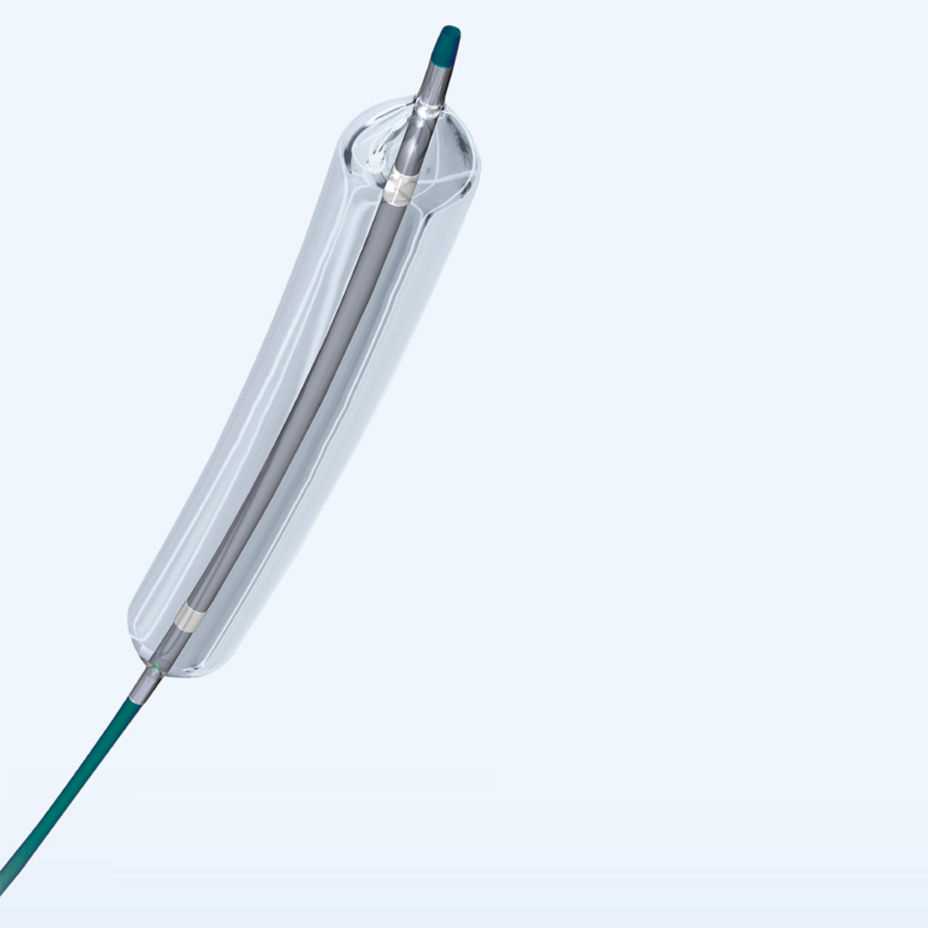
- Simultaneous deployment of Two covered stents in both common iliac arteries BEGRAFT(Bentley): 7x37mm il the right side & 7x27mm in the left side.
- Kissing balloon with the stent balloons.
- Angiographic control in different views with good inferior mesenteric artery patency.
- Bilateral femoral arteries manual compression.
Biobliography
-
2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS) - Article
Authors: Victor Aboyans, Jean-Baptiste Ricco, Marie-Louise E L Bartelink
Publication: [DOI: 10.1016/j.ejvs.2017.07.018
-
Authors: Taeymans K, Goverde P, Lauwers K, Verbruggen P.Publication: 2016 Jun;57(3):343-9. Epub 2016 Mar 24
-
Strategies for managing aortoiliac occlusions: access, treatment and outcomes - Article
Authors: Daniel G Clair, and Jocelyn M Beach
Publication: doi: [10.1586/14779072.2015.1036741]
-
A systematic review of endovascular treatment of extensive aortoiliac occlusive disease - Article
Authors: Vincent Jongkind & al.
Publication: doi.org/10.1016/j.jvs.2010.04.080
-
- Article
Authors : Beate Maria Stoeckelhuber & al.
Publication: J Vasc Interv Radiol 2003; 14:1443–1447
-
Long-term Results of Primary Stent Placement to Treat Infrarenal Aortic Stenosis - Article
Authors: P.C.G.Simons & al.
Publication: doi.org/10.1016/j.ejvs.2006.05.010
Date du tournage : 15/12/2017
Dernière mise à jour : 21/05/2021
Dernière mise à jour : 21/05/2021
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Partager
Participer à la discussion
Suggestions
Mardi 27 avril 2021 de 15h à 16h (GMT+2)
Honolulu : Mardi 27 avril 2021 de 03h à 04h (GMT+2)
San Francisco : Mardi 27 avril 2021 de 06h à 07h (GMT+2)
New York : Mardi 27 avril 2021 de 09h à 10h (GMT+2)
Buenos Aires : Mardi 27 avril 2021 de 10h à 11h (GMT+2)
Reykjavik : Mardi 27 avril 2021 de 13h à 14h (GMT+2)
London / Dublin : Mardi 27 avril 2021 de 14h à 15h (GMT+2)
Paris / Berlin : Mardi 27 avril 2021 de 15h à 16h (GMT+2)
Istanbul : Mardi 27 avril 2021 de 16h à 17h (GMT+2)
Moscou / Dubaï : Mardi 27 avril 2021 de 17h à 18h (GMT+2)
Bangkok : Mardi 27 avril 2021 de 20h à 21h (GMT+2)
Shanghai : Mardi 27 avril 2021 de 21h à 22h (GMT+2)
Tokyo : Mardi 27 avril 2021 de 22h à 23h (GMT+2)
Sydney : Mercredi 28 avril 2021 de 00h à 01h (GMT+2)
Wellington : Mercredi 28 avril 2021 de 02h à 03h (GMT+2)
San Francisco : Mardi 27 avril 2021 de 06h à 07h (GMT+2)
New York : Mardi 27 avril 2021 de 09h à 10h (GMT+2)
Buenos Aires : Mardi 27 avril 2021 de 10h à 11h (GMT+2)
Reykjavik : Mardi 27 avril 2021 de 13h à 14h (GMT+2)
London / Dublin : Mardi 27 avril 2021 de 14h à 15h (GMT+2)
Paris / Berlin : Mardi 27 avril 2021 de 15h à 16h (GMT+2)
Istanbul : Mardi 27 avril 2021 de 16h à 17h (GMT+2)
Moscou / Dubaï : Mardi 27 avril 2021 de 17h à 18h (GMT+2)
Bangkok : Mardi 27 avril 2021 de 20h à 21h (GMT+2)
Shanghai : Mardi 27 avril 2021 de 21h à 22h (GMT+2)
Tokyo : Mardi 27 avril 2021 de 22h à 23h (GMT+2)
Sydney : Mercredi 28 avril 2021 de 00h à 01h (GMT+2)
Wellington : Mercredi 28 avril 2021 de 02h à 03h (GMT+2)
Preserving Coronary Access After TAVI
Case of the month: September 2021
Partager
Complex Acute Anterior STEMI with "no Reflow phenomenon" management
Case of the month: October 2018
Partager
Occluded instent left SFA stenosis | Fractured stents treated - Eluvia stenting
Case of the month: June 2022
Partager
TEVAR of the thoracic aneurysm with short neck below left common carotid artery using C TAG with act...
Case of the month: March 2022
Partager




sadananda S. is the covered stent from right side behind the Aortic stent? since you did not remove the wire and re enter the lumen of aortic stent
Ahmed B. of course the right iliac covered stent is inside the aortic stent, the right iliac guidewire was unjailed just after the aortic stenting!!
Oğuz A. Dear Max Armor
Did you re-cross the first stent after removing initial wire and did you apply minimal protrusion into the first distal aortic stent. Were all wires 0.035 hydrophilic?
Ahmed B. Dear Ogus,
of course the right guidewire was unjailed just after the aortic stenting, the used guidewires are hydrophilic adventage 0.035 from Terumo
Oğuz A. Dear Max Amor
what was the lenght of both long sheats? And what is your opnion about the diastal aprtic residual plaque, it was behind the stent or inside? What is the follow-up strategy about this hazy plaque view?
Best regards
Oguz Akkus
Max A. The introducers that i have used were : left 7F 23cm with distal marker & 6F 23cm right .the distal plaque was covered by both stents (aortic and iliac ).
thank you for your comment!!
José P. Merci
Max A. you are welcome
Casals P. Fantastic
Max A. thank you !
Rajinikanth R. Why not 'uncovered' stents in the iliac arteries as well?
Ahmed B. we have prefered using covered stents to ensure well expansion in such calcified iliac lesions & overcome the risk of rupture !!
Maher J. Nice results
Max A. thank you
Mangesh T. Very well done case of Distal Aortic stenting with bilateral Common Iliac arterial balloon expandable covered stents deployment!!
My questions-
1.Since Aortic calcifications are Egg shell, cracking type with immediate danger of rupturing Aorta at bifurcation.
Hence why not deployed 'Covered stent' in Aorta?
Preserving Inferior Messentric Artery (IMA) was also possible with Covered stent like "Fluency plus" from BD-BARD.
2.I feel that it's "Sinus-Repo-Visual" Closed cell design 6F stent of size (12x40mm) and Not Sinus-XL 6F from Optimed.
All Sinus-XL Stents available in 14 & 16mm diameter. While Repo-Visual has 6-14mm diameter and 30-80 mm length.
Specially designed for "Highly calcified stenosis in straight vessel".
3.What was pressure for-Balloon inflation,Stent deployment, Post stent dilatation on inflation device?
4. Does Covered stent has Arterial vessel wall fixation ability, Anti-jump/migration features and high radial force?
5. Have you started some medicinal management for high blood pressure , severe claudications, cessation of smoking etc?
Am I correct? What is your opinion?
Ahmed B. Dear Mangesh,
thank you for these interesting questions,
1.usually we implant covered stent in such calcified aortic lesion, but in this particular case the IMA take-off is very close to the lesion (3mm) so the risk of occlusion is very high , we have prefered a non-covered one,
2.of course the aortic Stent is a Sinus-Repo-Visual 12x40mm.
3.for aortic predilatation : we have performed very carefull inflation & postdilatation at 8ATM. for the iliac stents the balloons were inflated as shown sequentially & then in kissing fashion at nominal pressure at 10 ATM.
4.yes we implant regulary this covered stent in our daily practice in different scenarios ( calcified lesions , emergent settings : traumatic & iatrogenic perforations , FA closure), we don't have a particular concerns regarding stability and radial force, have you any experience with this covered stent ?
5.of course the first step in the managment of our LEAD patients is optimal medical therpy & cardiovascular risk factors control .
can you tell as about you practice to approach such lesions ? prefered materials?
Ahmed B. Ce commentaire à été modéré
Ahmed B. Ce commentaire à été modéré
Kamran Z. Very nice case!
Do you need to oversize the sinus xl?
Does it depend on the extent of calcium or the result after predilation wheather you oversize?
Ahmed B. thank you Kamran!
it is a Sinus REpo-visual and not XL,
the stent was selected on the CT Scann measures (aortic dimension)
during the procedure, there were no oversizing and the kissing with nominal pressure is performed with balloons just in front of carina, so they don't protrude significantly in distal aorta !
this kissing stenting (covered stents) was performed to cover the distal aorta as well as the two iliac ositium !
you are welcome
Kamran Z. Thank you for the fast answer! Do you use Sinus xl for similar cases with greater diameter of the aorta (>14mm) when Repro is not suitable?
Ahmed B. Yes of course, we use the XL when diameter is greater !
Kambiz S. Excellent