×
Il semble que vous utilisiez une version obsolète de internet explorer. Internet explorer n'est plus supporté par Microsoft depuis fin 2015. Nous vous invitons à utiliser un navigateur plus récent tel que Firefox, Google Chrome ou Microsoft Edge.

Devenez membre d'Incathlab et bénéficiez d'un accès complet !
Vous devez être membre pour accéder aux vidéos Incathlab sans limitation. Inscrivez vous gratuitement en moins d'une minute et accédez à tous les services Incathlab ! Vous avez aussi la possibilité de vous connecter directement avec votre compte facebook ou twitter en cliquant sur login en haut à droite du site.
Inscription Connexion
Inscription Connexion
15777 vues
Case summary
- 49 Years old male
- Risk factors : HBP, smoker.
- Medical history : ischemic heart disease with PCI (LAD, RCA), lowerlimb artery disease with angioplasty (right iliac(2014 ASSURANT COBALT) and FSA (2010 MARIS), left FSA (2014 INNOVA) and popliteal artery (2014 PROMUS)).
- Clinical symptoms : intermittent claudication stage 2b
- Biological parameters : serum creatinine 8,2mg
- On going treatement : aspirin, ticagrelor, bisoprolol, ramipril, rosuvastatin.
Strategy
- Controlateral right femoral access
- 6 Fr braided catheter
- Management of common femoral
- Left superficial femoral artery angioplasty
Diagnostic images
This didactic procedure concerns a 49 years old man with a history of:
- Ischemic heart disease with PCI (LAD, RCA)
- Lower limb artery disease with multiple angioplasties: right iliac in 2014 (ASSURANT COBALT), right SFA in 2010 (MARIS), left SFA in 2014 (INNOVA) and right popliteal artery in 2014 (PROMUS).
Cardiovascular risk factors: Hypertension and smoking.
Actual treatments: Aspirin, Ticagrelor, Bisoprolol, Ramipril and Rosuvastatin.
He is presenting with severe left lower limb claudication with rest pain (stage3), (left > right). Several stents implanted on the left SFA 7 years ago.
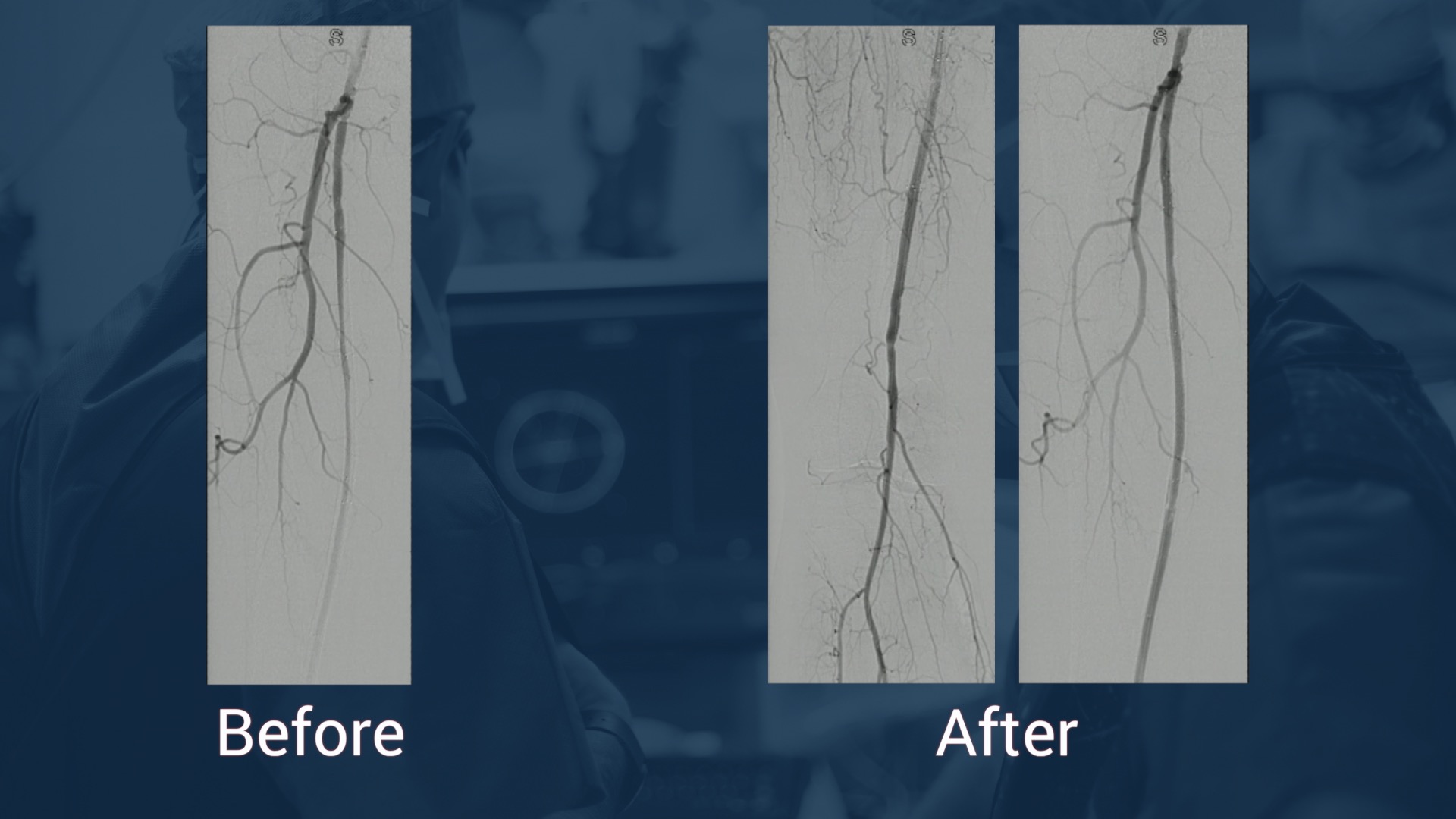
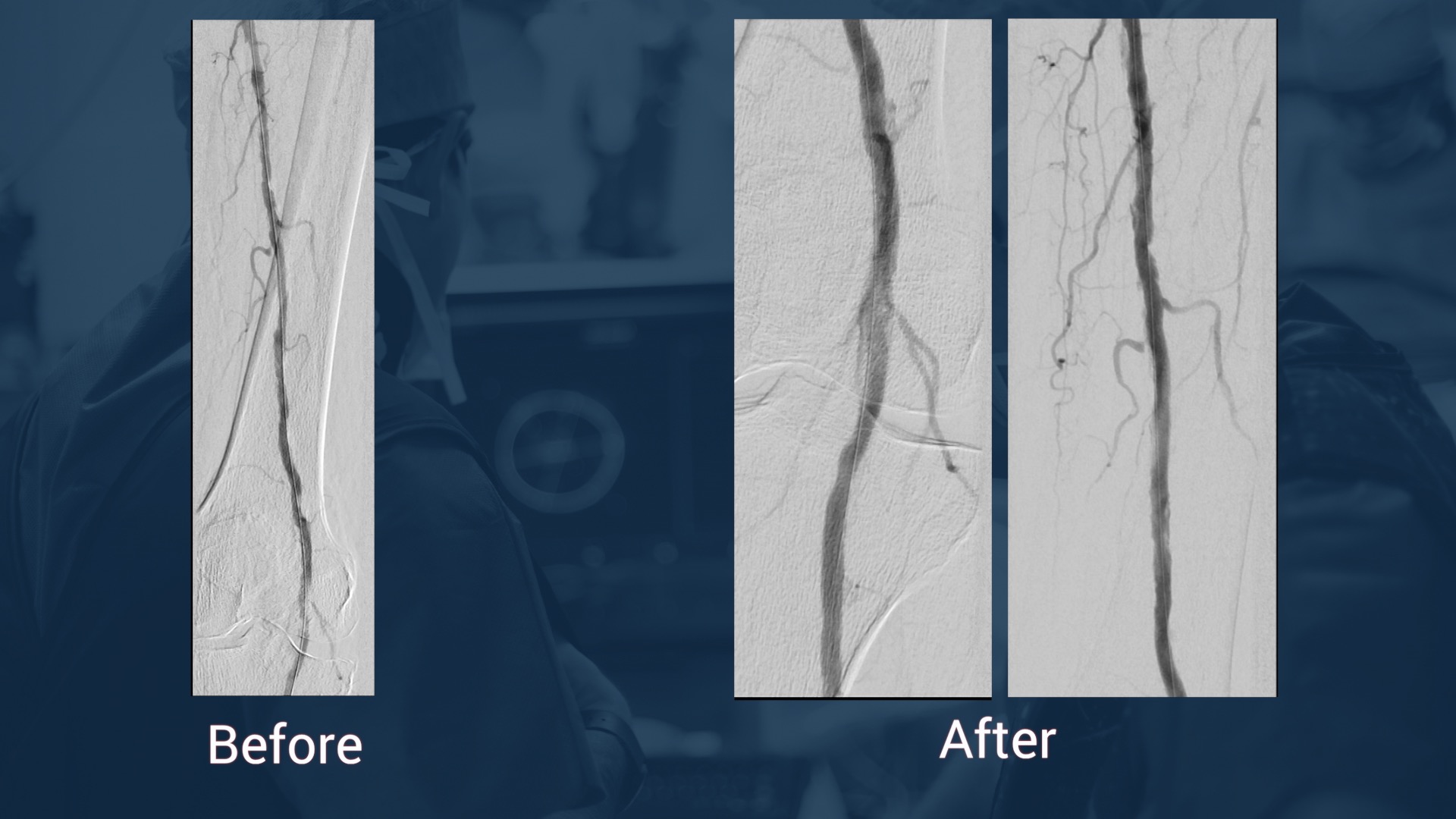
The angiographic control showed bilateral long SFA occlusions with stent fractures on the left SFA stents, and a left CFA stenosis.
Educationnel Objectives
- Plan a step-by-step SFA occlusion revascularization through contralateral access.
- Materials choice: guidewires, support catheter, sheath, balloons and stents.
- How to manage contralateral access.
- Instent restenosis: Stent fracture.
- Discuss therapeutic options.
- Lesion preparation in instent restenosis cases.
- How to perform an Innova stent deployment?
- How to achieve a good positioning and post dilatation of the stent?
- Tips and tricks for managing multiple lesions on the same axis (CFA and SFA)
- What are adjunctive pharmacotherapies?
Step-by-step procedure: SFA instent occlusion revascularization
- Access sites and cross over:
- Retrograde contralateral femoral access: Puncture under fluoroscopy with micro-puncture system, then a 6 French femoral sheath is positioned.
- Cross over with Reuter 5 French catheter and 0.035” GLIDEWIRE ADVANTAGE wire.
- Gentle crossing of the lesion of the left CFA stenosis.
- Exchange and advancing of a 6 Fr Flexor® introducer 45cm to the end of the left CFA
- Particular attention: The extremity of the introducer should be above the ostium of PFA for optimal imaging through collateral vascularization.
- Recanalization:
- Support catheter Berenstein with 0.035” GLIDEWIRE ADVANTAGE advanced through the occlusion with knuckled tip.
- The wire position should be “instent” through the occlusion: orthogonal views is useful to confirm that position.
- Externalization of the wire distally: be sur that the wire is knuckled to avoid distal vessel perforation.
- Predilatation
- Multiple predilatations of the fractured stents with a Mustang™ PTA Balloon 5*100mm.
- Multiple predilatations with a larger Mustang™ PTA Balloon 6*100mm at high pressure.
- Angiographic and fluoroscopic control of good stent expansion and antegrade flow.
- Careful positioning of the Stents covering the entry point of the occlusion and the distality of the occlusion.
- Stenting with Eluvia™ Drug-Eluting stent 6*150 mm, 7*150mm and 7*80mm.
- Post dilatation to ensure good stent apposition with Mustang™ PTA Balloon 6*100mm at high pressure.
- Angiographic control: checking for dissection and distal embolization.
- Flexion angiographic control: Knee flexion at 90°.
- Treatment of the lesion of the left CFA
- Direct stenting of the short lesion of the left CFA with a balloon expandable stent 7*18mm sized 1:1 with the artery with no over expansion to avoid dissection.
- Angiographic control
- 10)Medical adjunctive treatments
- Pre-procedural: Heparin and mild sedation.
- Post procedural: The patient is already under Aspirin, Ticagrelor and high statin dose for his ischemic heart disease.
Bibliography
-
Aboyans V, Ricco J-B, Bartelink M-LEL, Björck M, Brodmann M, Cohnert T, et al. 2017 ESC Guidelines on the Diagnosis and Treatment of Peripheral Arterial Diseases, in collaboration with the European Society for Vascular Surgery (ESVS). Eur Heart J. 1 mars 2018;39(9):763‑816.
https://pubmed.ncbi.nlm.nih.gov/28886620/
-
Gray WA, Keirse K, Soga Y, Benko A, Babaev A, Yokoi Y, et al. A polymer-coated, paclitaxel-eluting stent (Eluvia) versus a polymer-free, paclitaxel-coated stent (Zilver PTX) for endovascular femoropopliteal intervention (IMPERIAL): a randomised, non-inferiority trial. The Lancet. oct 2018;392(10157):1541‑51.
https://linkinghub.elsevier.com/retrieve/pii/S0140673618322621
-
Müller-Hülsbeck S, Benko A, Soga Y, Fujihara M, Iida O, Babaev A, et al. Two-Year Efficacy and Safety Results from the IMPERIAL Randomized Study of the Eluvia Polymer-Coated Drug-Eluting Stent and the Zilver PTX Polymer-free Drug-Coated Stent. Cardiovasc Intervent Radiol. mars 2021;44(3):368‑75.
https://link.springer.com/10.1007/s00270-020-02693-1
-
Müller-Hülsbeck S, Keirse K, Zeller T, Schroë H, Diaz-Cartelle J. Twelve-Month Results From the MAJESTIC Trial of the Eluvia Paclitaxel-Eluting Stent for Treatment of Obstructive Femoropopliteal Disease. J Endovasc Ther. oct 2016;23(5):701‑7.
http://journals.sagepub.com/doi/10.1177/1526602816650206
- Giannopoulos S, Lyden SP, Bisdas T, Micari A, Parikh SA, Jaff MR, et al. Endovascular Intervention for the Treatment of Trans-Atlantic Inter-Society Consensus (TASC) D Femoropopliteal Lesions: A Systematic Review and Meta-Analysis. Cardiovasc Revasc Med. janv 2021;22:52‑65. https://pubmed.ncbi.nlm.nih.gov/32563709/
-
Niazi K, Tukaye DN. Challenges of Stent Restenosis in Superficial Femoral and Popliteal Artery Disease. JACC Cardiovasc Interv. oct 2017;10(20):2124‑5.
https://linkinghub.elsevier.com/retrieve/pii/S1936879817317879
-
Rymer JA, Jones WS. Femoropopliteal In-Stent Restenosis: What Is the Standard of Care? Circ Cardiovasc Interv [Internet]. déc 2018 [cité 25 févr 2022];11(12).
Disponible sur: https://www.ahajournals.org/doi/10.1161/CIRCINTERVENTIONS.118.007559
-
Yahagi K, Otsuka F, Sakakura K, Sanchez OD, Kutys R, Ladich E, et al. Pathophysiology of superficial femoral artery in-stent restenosis. J Cardiovasc Surg (Torino). juin 2014;55(3):307‑23.
PMID: 24755699
-
Neil N. Stent Fracture in the Superficial Femoral and Proximal Popliteal Arteries: Literature Summary and Economic Impacts. Perspect Vasc Surg Endovasc Ther. 1 juin 2013;25(1‑2):20‑7.
http://journals.sagepub.com/doi/ 10.1177/1531003513509122
Date du tournage : 13/07/2016
Dernière mise à jour : 03/06/2022
Dernière mise à jour : 03/06/2022
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Partager
Participer à la discussion
Suggestions
Complex Acute Anterior STEMI with "no Reflow phenomenon" management
Case of the month: October 2018
Partager
Nothing Left behind Strategy: Long SFA lesion, Directional atherectomy & DCB
Case of the month: December 2018
Partager




Aprigliano G. Of course you gained an immediate acceptable angiographic result. The patient is 50 yrs old, what should we attend from this procedure in terms of long term results? DES demonstrated to reduce long term restenosis in terms of intimal iperplasia but not in terms of stent fracture. May be interesting in this case another self expandable stent with unconventional design (Supera?). Thanks for sharin
Max A. We think that we can reduce the rate of restenosis .Best regards
Popeski P. .