
Devenez membre d'Incathlab et bénéficiez d'un accès complet !
Inscription Connexion
This month, we present the case of an 80 years old male patient, smoker, known to have HFrEF secondary to a cardiac amyloidosis TTR s/p CRT-D, severe aortic stenosis (ASA 0.6 cm2), hypertension, dyslipidemia and chronic kidney disease.
Coronary angiography pre-TAVR revealed: dominated RCA that is occluded as well as a moderate lesion of the obtuse marginal and severely calcified lesions of the proximal and mid LAD that is occluded distally.
Educational objectives
- How to manage a high-risk patient with multiple co-morbidities.
- Plan a step-by-step approach procedure for calcified lesion preparation and stenting.
- Choice of material: introducer size, guidewires, guide extension, choice of lesion modifying technique/tools.
- Role of intravascular imaging.
Step-by-step procedure:
1) Access site and hemodynamic stability:
- Right radial approach: 7 French EBU 3.5 to the left main.
- Under Dobutamine IV infusion.
- Anticoagulation using heparin.
2) Intravascular imaging:
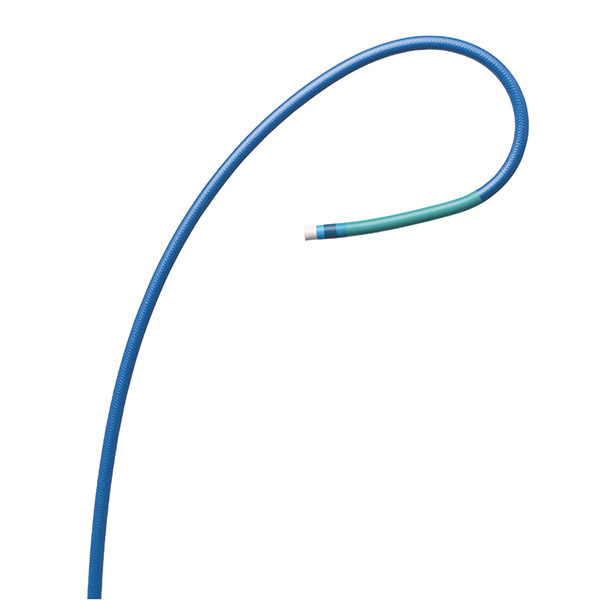
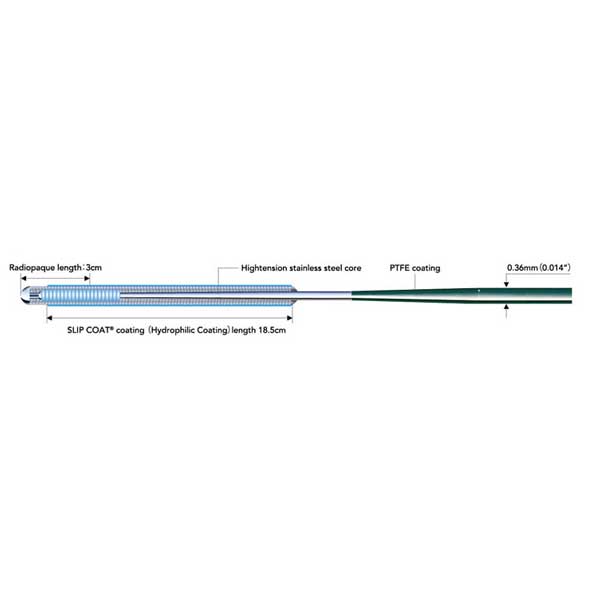
- Two 0.014” Sion Blue (Asahi) guidewires for extra support were introduced into the LAD.
- Intravascular imaging using optical frequency domain imaging (OFDI) (Terumo) at 40 mm/sec in order to minimize contrast injection showed superficially calcified LAD with several calcified nodules at the mid-LAD level and 360° calcium rings.
3) Calcium modifying device:
- Intravascular lithotripsy using a 3.5 x 12 mm Shockwave balloon was selected and the mid-LAD and proximal LAD lesions were predilated.
- Upon balloon inflations, a drop of blood pressure was noted, a small dose of Noradrenaline was set up.
- Further lesion preparation using a non-compliant balloon 3.5 mm inflated up to 20 atm was done at the level of the mid and proximal LAD lesions.
4) LAD stenting:
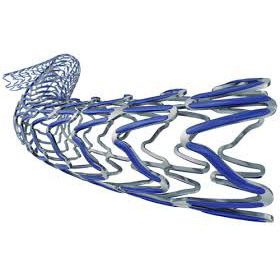
- A 3.5 x 21 mm Nagomi Ultimaster (Terumo) stent could not cross the proximal LAD lesion.
- A 6 French (due to out-of-stock 7 French) Boosting guide extension catheter (QX Medical) was introduced to the mid-LAD and facilitated stent delivery to the mid-LAD lesion that was inflated to 16 atm.
- Using the stent balloon, the guide extension catheter was advanced into the recently implanted stent.
- A 4.0 x 33 mm Nagomi Ultimaster (Terumo) was then implanted to cover the proximal LAD lesion and inflated to 16 atm.
5) Stent optimization:
- An OFDI run was performed at this time in order to assess the implanted stents and showed stent malapposition at different levels as well as a small dissection.
- Post-dilatation of the distal stent using a 4.0 mm non-compliant balloon inflated at 20 atm followed by a post-dilatation of the proximal stent using a 4.5 mm non-compliant balloon inflated at 20 atm were performed.
- The angiographic end-result was perfect.
6) Post-procedure patient care:
- Dobutamine tapering to stop over the next hour.
Bibliography
Dernière mise à jour : 22/03/2024
Live Case 4C 2023
6e Edition 4C 2023 JEUDI 21 SEPTEMBRE SESSION #1: L'OCT DANS LE STENTING FAILURE Modérateurs : Matthieu Godin & Nic...
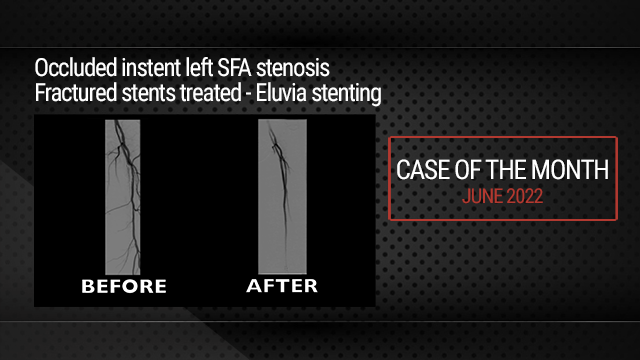
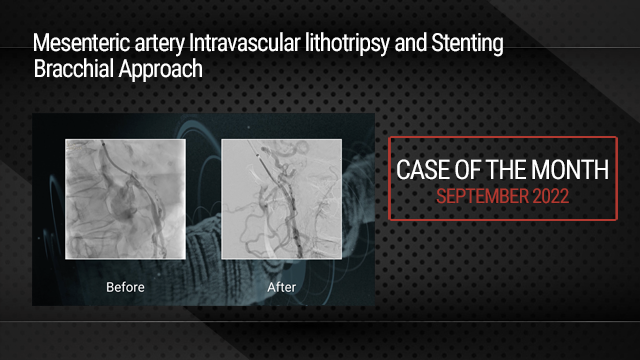
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Participer à la discussion
Suggestions
San Francisco : Lundi 29 novembre 1999 de 15h à 15h (GMT+1)
New York : Lundi 29 novembre 1999 de 18h à 18h (GMT+1)
Buenos Aires : Lundi 29 novembre 1999 de 20h à 20h (GMT+1)
London / Dublin : Lundi 29 novembre 1999 de 23h à 23h (GMT+1)
Paris / Berlin : Mardi 30 novembre 1999 de 00h à 00h (GMT+1)
Istanbul : Mardi 30 novembre 1999 de 01h à 01h (GMT+1)
Moscou / Dubaï : Mardi 30 novembre 1999 de 03h à 03h (GMT+1)
Bangkok : Mardi 30 novembre 1999 de 06h à 06h (GMT+1)
Shanghai : Mardi 30 novembre 1999 de 07h à 07h (GMT+1)
Tokyo : Mardi 30 novembre 1999 de 08h à 08h (GMT+1)
Sydney : Mardi 30 novembre 1999 de 09h à 09h (GMT+1)
Wellington : Mardi 30 novembre 1999 de 11h à 11h (GMT+1)



v22e V. visiteur2@altilab.com