×
Il semble que vous utilisiez une version obsolète de internet explorer. Internet explorer n'est plus supporté par Microsoft depuis fin 2015. Nous vous invitons à utiliser un navigateur plus récent tel que Firefox, Google Chrome ou Microsoft Edge.

Devenez membre d'Incathlab et bénéficiez d'un accès complet !
Vous devez être membre pour accéder aux vidéos Incathlab sans limitation. Inscrivez vous gratuitement en moins d'une minute et accédez à tous les services Incathlab ! Vous avez aussi la possibilité de vous connecter directement avec votre compte facebook ou twitter en cliquant sur login en haut à droite du site.
Inscription Connexion
Inscription Connexion
40851 vues
Program
| 12.30 | Introduction |
| 12.32 |
Overview of devices: ○ Veniti stent – Stephen Black ○ Wallstent – Olivier Hartung ○ IVUS – Peter Neglen |
| 12.47 |
Case in box n°1: May-Thurner syndrome Panel discussion |
| 12.57 |
Case in box n°2: May-Thurner syndrome Panel discussion |
| 13.07 |
Acute DVT: ○ Goals and history of clot removal strategies – Yves Alimi ○ PMT - Stephen Black |
| 13.25 |
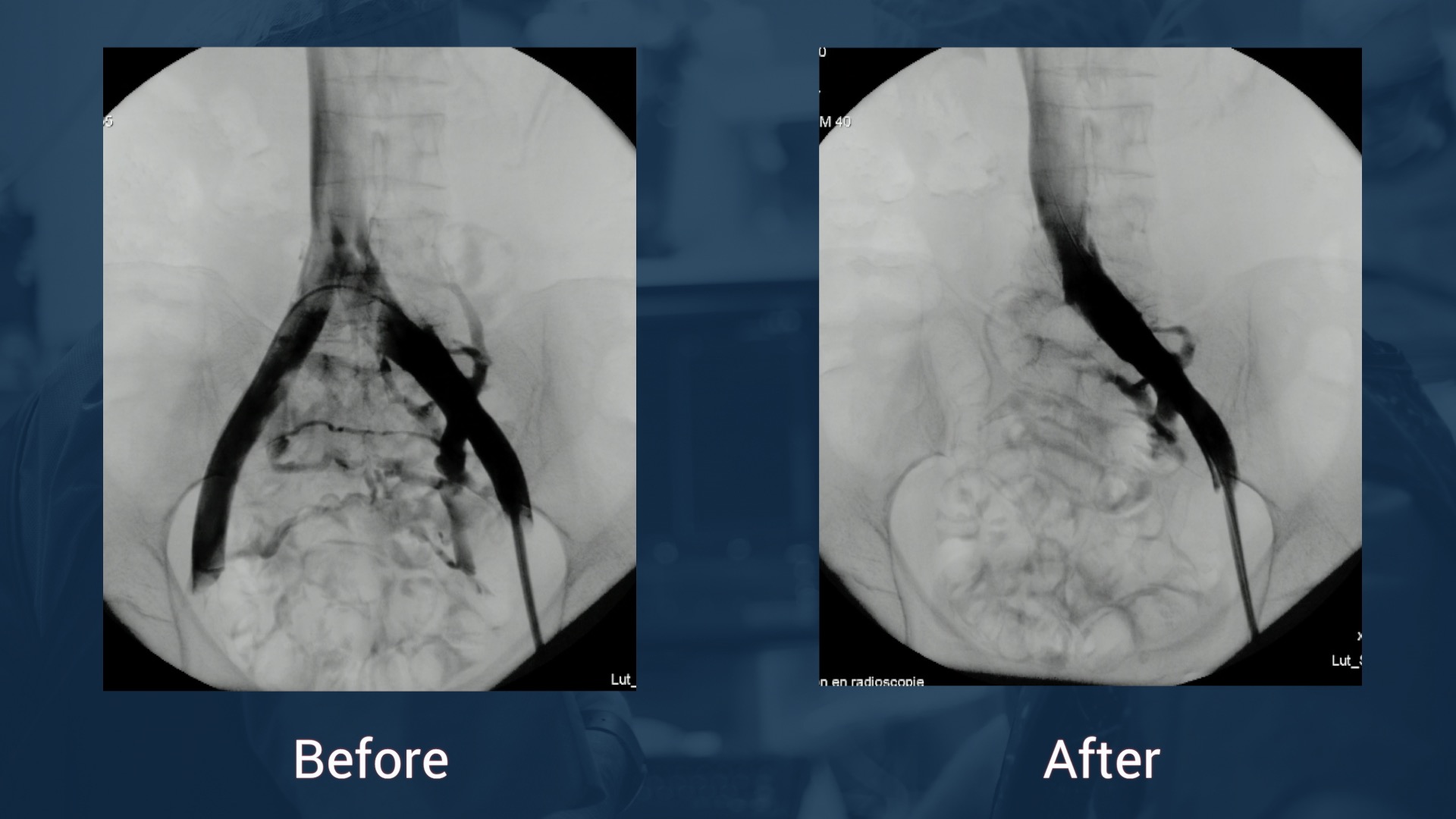
Treatment of chronic lesions: ○ Recanalization – Olivier Hartung |
| 13.33 |
Case in box n°3: Left femoro iliac vein recanalization and stenting Panel discussion |
| 13.41 |
Case in box n°4: Left femoro iliac vein recanalization and stenting Panel discussion |
| 13.55 | Conclusion |
Educational objectives
- Diagnostic approach for patients with suspected ilio-femoral vein obstructions
-
Tips and Tricks for venous recanalization in patients with:
- Acute DVT
- May Thurner Syndrome
- Chronic obstructions of the ilio-femoral vein system
- Stent design, performance and available evidence
- Value of Intravascular ultrasound (IVUS) for venous recanalizsation
Audience
- Endovascular specialists (Vascular Surgeons, Interventional Radiologists, Angiologists and Interventional Cardiologists) interested and/or specialized in venous interventions
- Referring physicians of patients with venous disease
Date du tournage : 13/10/2017
Dernière mise à jour : 26/06/2018
Dernière mise à jour : 26/06/2018
Participer à la discussion
Suggestions
Mercredi 24 juin 2020 de 18h à 19h30 (GMT+2)
Honolulu : Mercredi 24 juin 2020 de 07h à 08h30 (GMT+2)
San Francisco : Mercredi 24 juin 2020 de 10h à 11h30 (GMT+2)
New York : Mercredi 24 juin 2020 de 13h à 14h30 (GMT+2)
Buenos Aires : Mercredi 24 juin 2020 de 14h à 15h30 (GMT+2)
Reykjavik : Mercredi 24 juin 2020 de 17h à 18h30 (GMT+2)
London / Dublin : Mercredi 24 juin 2020 de 18h à 19h30 (GMT+2)
Paris / Berlin : Mercredi 24 juin 2020 de 19h à 20h30 (GMT+2)
Istanbul : Mercredi 24 juin 2020 de 20h à 21h30 (GMT+2)
Moscou / Dubaï : Mercredi 24 juin 2020 de 21h à 22h30 (GMT+2)
Bangkok : Jeudi 25 juin 2020 de 00h à 01h30 (GMT+2)
Shanghai : Jeudi 25 juin 2020 de 01h à 02h30 (GMT+2)
Tokyo : Jeudi 25 juin 2020 de 02h à 03h30 (GMT+2)
Sydney : Jeudi 25 juin 2020 de 04h à 05h30 (GMT+2)
Wellington : Jeudi 25 juin 2020 de 06h à 07h30 (GMT+2)
San Francisco : Mercredi 24 juin 2020 de 10h à 11h30 (GMT+2)
New York : Mercredi 24 juin 2020 de 13h à 14h30 (GMT+2)
Buenos Aires : Mercredi 24 juin 2020 de 14h à 15h30 (GMT+2)
Reykjavik : Mercredi 24 juin 2020 de 17h à 18h30 (GMT+2)
London / Dublin : Mercredi 24 juin 2020 de 18h à 19h30 (GMT+2)
Paris / Berlin : Mercredi 24 juin 2020 de 19h à 20h30 (GMT+2)
Istanbul : Mercredi 24 juin 2020 de 20h à 21h30 (GMT+2)
Moscou / Dubaï : Mercredi 24 juin 2020 de 21h à 22h30 (GMT+2)
Bangkok : Jeudi 25 juin 2020 de 00h à 01h30 (GMT+2)
Shanghai : Jeudi 25 juin 2020 de 01h à 02h30 (GMT+2)
Tokyo : Jeudi 25 juin 2020 de 02h à 03h30 (GMT+2)
Sydney : Jeudi 25 juin 2020 de 04h à 05h30 (GMT+2)
Wellington : Jeudi 25 juin 2020 de 06h à 07h30 (GMT+2)
CTO crossing and their challenges
Partager










Sharif Khashaba K. kindly improve the voice
Vanessa R. How do you treat venous non thrombotic in stent restenosis
Gustavo R. In chronic oclusion how often did you see instent stenosis in Iliocaval Wallstent
Olivier H. in our experience on 162 patients with a median follow-up of 44 months, primary patency is 70% at 60 months and assisted primary patency 85%
Peter N. Using the Wallstent, the cumulative in-stent stenosis rate at 6 years is in non-thrombotic obstructions (NIVL) 1% and in postthrombotic obstructions approximately 10%. In-stent stenosis is then defined as being >50% lumen reduction. It is common to see some in-stent layering of
Jacobo N. What do you think is the best aproach to the lesion, popliteal or contralateral? Thanks
Olivier H. for chronic lesion, i prefer anterograde approach through the femoral or popliteal. Some teams favor internal jugular approach (must always be ready in case of IVC lesions)
for acute lesions, it depends on the patency of the popliteal vein. If occluded, jugular or controlateral acess
Maria Fabrizia G. do you use the same strategy in presence of PE?
Olivier H. PE does not change the strategy but can make discuss the use of an IVC filter
bander A. what is he indications in case of non thrombotic iliac vein lesion ?
Olivier H. symptomatic and disabled patients C2-6, pelvic congestion syndrome
Peter N. I agree with Olivier, but wants to qualify it slightly. As we pointed out in the discussion, compression of the iliac veins are common in the asymptomatic population and possibly up to 30% have >50% stenosis with no symptoms! So there is a potential risk of overtreatment. In chronic venous disease of the lower limb, treatment of the outflow obstruction is indicated in patients with the C-class in CEAP being marked swelling (C3) and those with skin changes/ulcers (C4-C6). In addition, you have those patients with venous pain without skin changes or varicose veins, which can not be solely explained by the presence of reflux, if any. We use visual analogue scale (VAS) to evaluate that, considering VAS >5 being significant. As Olivier pointed out the symptoms have to affect the patients' quality of life.
Sandeep S. When using three stents, why is the middle stent placed last in iliofemoral venous intervention?
Is there any algorithim to decide on when and not to stent across deep femoral vein?