×
It looks like you're using an obsolete version of internet explorer. Internet explorer is no longer supported by Microsoft since the end of 2015. We invite you to use a newer browser such as Firefox, Google Chrome or Microsoft Edge.
My Player placeholder

Become an Incathlab member and receive full access to its content!
You must be an Incathlab member to access videos without any restrictions. Register for free in one minute and access all services provided by Incathlab.You will also be able to log into Incathlab from your Facebook or twitter account by clicking on login on the top-right corner of Incathlab website.
Registration Login
Registration Login
This didactic procedure regards a 60 years old man presenting a severe left lower limb claudication with rest pain (stage 3). The patient has a history of two femoro-infrapopliteal venous bypasses which both occluded shortly after. Multimodality imaging revealed a long occlusion of the femoropopliteal axis with a severely diseased posterior tibial artery. A previous antegrade attempt of recanalization failed due to severe calcification. No retrograde attempt was done due to severe claudication. The patient has finally undergone a percutaneous femoropopliteal bypass.
Educational objectives
- Define the indication of percutaneous femoro-popliteal bypass (PFPB) in severe lower limb disease.
- Plan a step-by-step procedure of PFBP.
- How to manage antegrade and retrograde access?
- How to choose the accurate spots for the implantation of PFPB: proximal and distal implantation.
- Selecting the appropriate devices : guidewires, microcatheters, guiding catheter, balloons and covered stents
- How to modify a guiding catheter for a coaxial transseptal needle system?
- How to safely perform a puncture using transseptal needle through occluded femoral artery.
- How to safely perform an externalization and extra-vessel trajectory?
- Tips and tricks to a successful puncture and reentry.
- What are adjunctive pharmacotherapies?
Step-by-step procedure: supra-articular femoropopliteal percutaneous bypass
1) Access sites:
- Antegrade femoral access: 6 French sheath and 8 French sheath for final stenting.
- Retrograde access through the anterior tibial artery (ATA).
2) Retrograde recanalization:
- V-18™ wire and Terumo 0.035” angled stiff Glidewire® with the support of TrailBlazer™ microcatheter.
- Advancement of knuckled wire through tibioperoneal trunk (TPT) subintimally until the landing zone (distal third of left superficial femoral artery (FSA))
- Pre-dilatation: OTW Armada balloons : 3*60 mm then 5*60 mm.
3) Preparation of the landing zone:
- Predilatation: OTW Armada balloon 5*60 mm.
- Use the balloon in place to identify the landing zone..
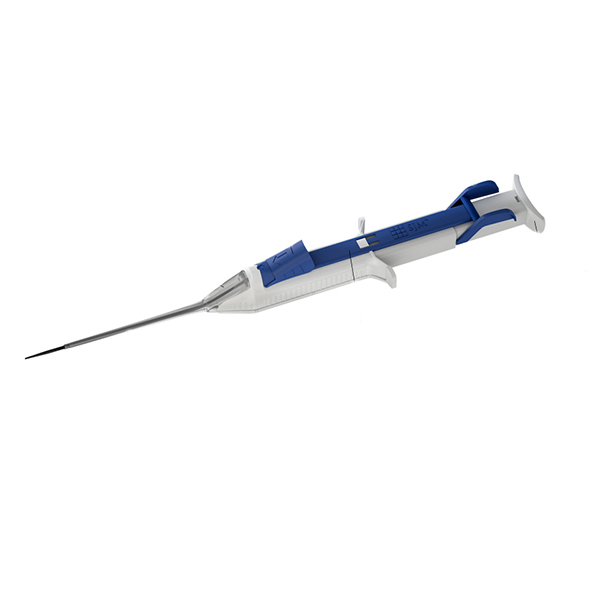
4) Preparation of the transseptal needle:
- 6 French guiding catheter cut to obtain a shorter one at the level of the transseptal needle curve
- Insertion of the transseptal needle in the modified 6 French guiding catheter to protect the needle (avoid vessel perforation or dissection).
- Coaxial system: direct the transseptal needle and puncture safely.
5) Externalisation and extravessel trajectory :
- Puncture of the vessel wall toward the medial side of the proximal cap of the occluded vessel (avoid collateral vessels).
- Injection of diluted Lidocaïne (0.1%) locally.
- Advancement of the knuckled Terumo 0.035’’ angled Glidewire® into the extravascular space, paralleled to the native vessel (following calcifications) with the support of the guiding catheter.
6) Reentry
- Balloon dilatation from retrograde access at the reentry site (REVERSE CART technique).
- Puncture at the reentry site: balloon and guidewire from retrograde access serve as a benchmark, and orthogonal views.
- Pre-dilatation of the reentry site: Armada OTW balloon 4*60 mm
- Positioning of the guiding catheter downstream to the reentry site, inside the vessel structure.
7) Stenting:
- Exchange to a support guidewire: Lunderquist Extra Stiff 0.035’’ guidewire.
- Exchange to an 8 French sheath 45cm which is advanced downstream to the distal reentry point.
- Stenting the reentry point: Covera™ stent 6*100 mm.
- Stenting the extra-vessel trajectory: Viabahn®7*150 mm with long overlapping.
- Stenting the exit point Viabahn® 7*80 mm with long overlapping.
8) Antegrade angioplasty:
- Predilatation and stenting of the popliteal artery.
- Remove ATA sheath and balloon hemostasis.
9) Post dilatation of the covered stents
10) Medical adjunctive treatments
- Pre-procedural: Heparin and Antibioprophylaxis.
- Post procedural: Triple therapy: Aspirin 75mg o.d. + Clopidogrel 75mg o.d. + Enoxaparin 100 UI/kg b.i.d. : 15 days.
- DUS 15 days after.
- Stop Clopidogrel and continue Aspirin 75mg b.i.d and NAOC.
Bibliography
Procedure
- Procedure time: 105 min
- Exposure time: 44 min
- Exposure: 190 mGy
- Contrast volume: 100 ml Visipaque 320
Shooting date : 2019-11-08
Last update : 2021-05-11
Last update : 2021-05-11
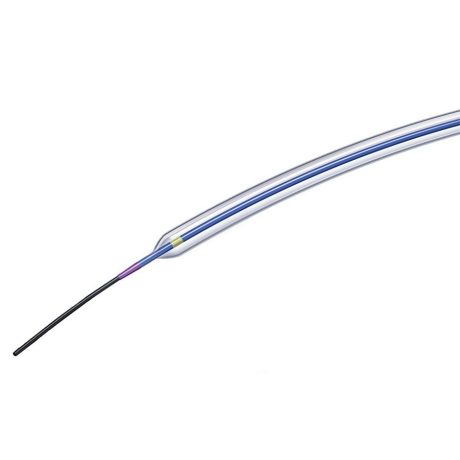
Sterling™ PTA Balloon dilatation catheter / Boston Scientific
PTA Balloon dilatation catheter
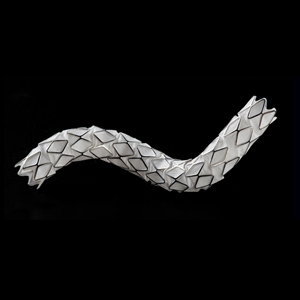
GORE® VIABAHN® VBX Balloon Expandable Endoprosthesis / Gore
Flexible strength. Proven success.
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Share
Suggestions
Discover your Monthly Case
Honolulu : Sunday, September 17th 2023 from 09:07pm to 09:07pm (GMT+2)
San Francisco : Monday, September 18th 2023 from 12:07am to 12:07am (GMT+2)
New York : Monday, September 18th 2023 from 03:07am to 03:07am (GMT+2)
Buenos Aires : Monday, September 18th 2023 from 04:07am to 04:07am (GMT+2)
Reykjavik : Monday, September 18th 2023 from 07:07am to 07:07am (GMT+2)
London / Dublin : Monday, September 18th 2023 from 08:07am to 08:07am (GMT+2)
Paris / Berlin : Monday, September 18th 2023 from 09:07am to 09:07am (GMT+2)
Istanbul : Monday, September 18th 2023 from 10:07am to 10:07am (GMT+2)
Moscou / Dubaï : Monday, September 18th 2023 from 11:07am to 11:07am (GMT+2)
Bangkok : Monday, September 18th 2023 from 02:07pm to 02:07pm (GMT+2)
Shanghai : Monday, September 18th 2023 from 03:07pm to 03:07pm (GMT+2)
Tokyo : Monday, September 18th 2023 from 04:07pm to 04:07pm (GMT+2)
Sydney : Monday, September 18th 2023 from 06:07pm to 06:07pm (GMT+2)
Wellington : Monday, September 18th 2023 from 08:07pm to 08:07pm (GMT+2)
San Francisco : Monday, September 18th 2023 from 12:07am to 12:07am (GMT+2)
New York : Monday, September 18th 2023 from 03:07am to 03:07am (GMT+2)
Buenos Aires : Monday, September 18th 2023 from 04:07am to 04:07am (GMT+2)
Reykjavik : Monday, September 18th 2023 from 07:07am to 07:07am (GMT+2)
London / Dublin : Monday, September 18th 2023 from 08:07am to 08:07am (GMT+2)
Paris / Berlin : Monday, September 18th 2023 from 09:07am to 09:07am (GMT+2)
Istanbul : Monday, September 18th 2023 from 10:07am to 10:07am (GMT+2)
Moscou / Dubaï : Monday, September 18th 2023 from 11:07am to 11:07am (GMT+2)
Bangkok : Monday, September 18th 2023 from 02:07pm to 02:07pm (GMT+2)
Shanghai : Monday, September 18th 2023 from 03:07pm to 03:07pm (GMT+2)
Tokyo : Monday, September 18th 2023 from 04:07pm to 04:07pm (GMT+2)
Sydney : Monday, September 18th 2023 from 06:07pm to 06:07pm (GMT+2)
Wellington : Monday, September 18th 2023 from 08:07pm to 08:07pm (GMT+2)
Complex multivascular patient with occluded brachiocephalic trunk
Case of the month: September 2023
Share
Complex Ostial LAD CTO: Saphenous vein Graft as an Option for Retrograde Approach
Case of the month: July 2019 - Live case #7 ML CTO
Share
Calcified distal Left Main and LAD stenoses - Rotablation treatment and IVUS evalutation
Case of the month: June 2017
Share