×
It looks like you're using an obsolete version of internet explorer. Internet explorer is no longer supported by Microsoft since the end of 2015. We invite you to use a newer browser such as Firefox, Google Chrome or Microsoft Edge.
My Player placeholder

Become an Incathlab member and receive full access to its content!
You must be an Incathlab member to access videos without any restrictions. Register for free in one minute and access all services provided by Incathlab.You will also be able to log into Incathlab from your Facebook or twitter account by clicking on login on the top-right corner of Incathlab website.
Registration Login
Registration Login
39867 views
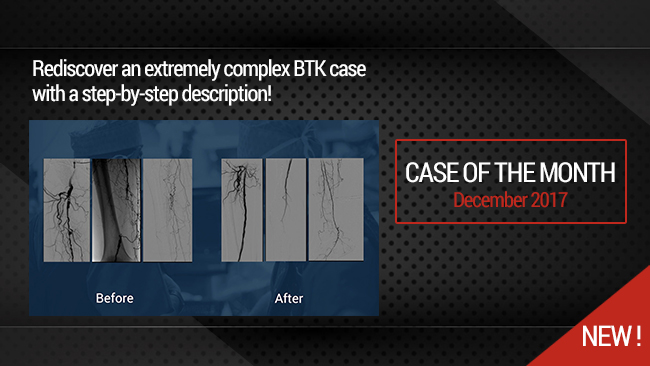
This 18 minutes didactic procedure concerns a 78 years old male with extremely severe peripheral artery disease: a Left limb amputation and a Right limb trophic ulcer. He presents Three right consecutive artery occlusions: Mid-SFA, Popliteal, proximal and distal posterior tibial.
This extremely complex case was treated using different technics according to the arterial segment: Sub intimal angioplasty and long stenting for SFA, Drug coated balloon for Popliteal, DES for proximal posterior tibial and coronary technics for plantar arteries.
Step-by-Step Procedure
- Right Antegrade femoral access
- Pre-procedure discussion of strategy for a multilevel artery occlusion
- Guide wire selection and escalation for crossing
- Support micro-catheter selection
- Pre-dilatation of more than 50cm with low profile long balloon
- Technics to re--enter in foot arteries
- DES for distal leg arteries
- DCB for popliteal artery
- Self-expandable drug eluting stent for dissection and residual stenosis of SFA
Learning points
- Selection and feasibility of antegrade femoral access
- Guide Wire and micro-catheter selection for multilevel crossing
- Balloon angioplasty with low profile long balloons
- Technics to re-enter in plantar artery
- Use of DCB (Drug Coated Balloon) for popliteal artery
- Use of balloon DES in tibial artery
- Self -expandable DES at the femoral level
Biobliography
-
Short-Term Results of Eluvia™ Paclitaxel-Eluting Stent in External Iliac and Femoropopliteal Lesions - Article
Elens M, Verhelst R, Possoz J, Mastrobuoni S, Lacroix V, Astarci P.
Surg Technol Int. 2017 Nov 9;31. pii: sti31/894. [Epub ahead of print]
-
Drug-coated balloon angioplasty for the management of recurring infrapopliteal disease in diabetic patients with critical limb ischemia - Article
Palena LM, Diaz-Sandoval LJ, Gòmez Jabalera E, Peypoch Perez O, Sultato E, Brigato C, Brocco E, Manzi M.
Cardiovasc Revasc Med. 2017 Jun 20. pii: S1553-8389(17)30196-3. doi: 10.1016/j.carrev.2017.06.006. [Epub ahead of print]
-
Innovations in the Endovascular Management of Critical Limb Ischemia: Retrograde Tibiopedal Access and Advanced Percutaneous Techniques - Article
Mustapha JA, Diaz-Sandoval LJ, Saab F.
Curr Cardiol Rep. 2017 Aug;19(8):68. doi: 10.1007/s11886-017-0879-1.
-
Innovations in the Endovascular Management of Critical Limb Ischemia: Retrograde Tibiopedal Access and Advanced Percutaneous Techniques - Article
Mustapha JA, Diaz-Sandoval LJ, Saab F.
Curr Cardiol Rep. 2017 Aug;19(8):68. doi: 10.1007/s11886-017-0879-1.
-
Angiosome-directed revascularization in patients with critical limb ischemia - Article
Jongsma H, Bekken JA, Akkersdijk GP, Hoeks SE, Verhagen HJ, Fioole B.
J Vasc Surg. 2017 Apr;65(4):1208-1219.e1. doi: 10.1016/j.jvs.2016.10.100.
Shooting date : 2016-12-05
Last update : 2018-01-31
Last update : 2018-01-31
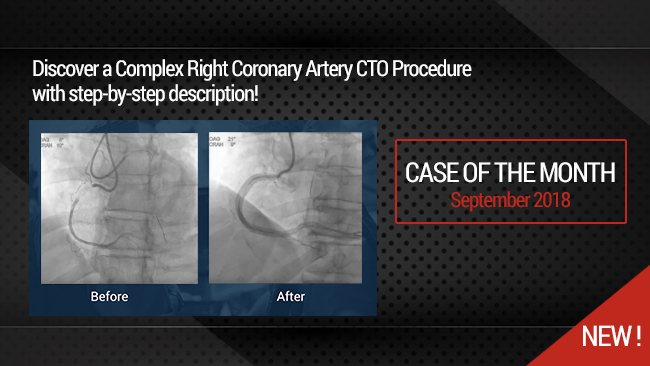
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Share
Join the Discussion
Suggestions
May 2017
Honolulu : Tuesday, May 9th 2017 from 12:30am to 02am (GMT+2)
San Francisco : Tuesday, May 9th 2017 from 03:30am to 05am (GMT+2)
New York : Tuesday, May 9th 2017 from 06:30am to 08am (GMT+2)
Buenos Aires : Tuesday, May 9th 2017 from 07:30am to 09am (GMT+2)
Reykjavik : Tuesday, May 9th 2017 from 10:30am to 12pm (GMT+2)
London / Dublin : Tuesday, May 9th 2017 from 11:30am to 01pm (GMT+2)
Paris / Berlin : Tuesday, May 9th 2017 from 12:30pm to 02pm (GMT+2)
Istanbul : Tuesday, May 9th 2017 from 01:30pm to 03pm (GMT+2)
Moscou / Dubaï : Tuesday, May 9th 2017 from 02:30pm to 04pm (GMT+2)
Bangkok : Tuesday, May 9th 2017 from 05:30pm to 07pm (GMT+2)
Shanghai : Tuesday, May 9th 2017 from 06:30pm to 08pm (GMT+2)
Tokyo : Tuesday, May 9th 2017 from 07:30pm to 09pm (GMT+2)
Sydney : Tuesday, May 9th 2017 from 09:30pm to 11pm (GMT+2)
Wellington : Tuesday, May 9th 2017 from 11:30pm to 01am (GMT+2)
San Francisco : Tuesday, May 9th 2017 from 03:30am to 05am (GMT+2)
New York : Tuesday, May 9th 2017 from 06:30am to 08am (GMT+2)
Buenos Aires : Tuesday, May 9th 2017 from 07:30am to 09am (GMT+2)
Reykjavik : Tuesday, May 9th 2017 from 10:30am to 12pm (GMT+2)
London / Dublin : Tuesday, May 9th 2017 from 11:30am to 01pm (GMT+2)
Paris / Berlin : Tuesday, May 9th 2017 from 12:30pm to 02pm (GMT+2)
Istanbul : Tuesday, May 9th 2017 from 01:30pm to 03pm (GMT+2)
Moscou / Dubaï : Tuesday, May 9th 2017 from 02:30pm to 04pm (GMT+2)
Bangkok : Tuesday, May 9th 2017 from 05:30pm to 07pm (GMT+2)
Shanghai : Tuesday, May 9th 2017 from 06:30pm to 08pm (GMT+2)
Tokyo : Tuesday, May 9th 2017 from 07:30pm to 09pm (GMT+2)
Sydney : Tuesday, May 9th 2017 from 09:30pm to 11pm (GMT+2)
Wellington : Tuesday, May 9th 2017 from 11:30pm to 01am (GMT+2)
DCB or DES: I want choice (Live session)
Updated algorithm for your daily practice
Share
Thursday, September 7th 2017 from 12pm to 01:30pm (GMT+2)
Honolulu : Thursday, September 7th 2017 from 01am to 02:30am (GMT+2)
San Francisco : Thursday, September 7th 2017 from 04am to 05:30am (GMT+2)
New York : Thursday, September 7th 2017 from 07am to 08:30am (GMT+2)
Buenos Aires : Thursday, September 7th 2017 from 08am to 09:30am (GMT+2)
Reykjavik : Thursday, September 7th 2017 from 11am to 12:30pm (GMT+2)
London / Dublin : Thursday, September 7th 2017 from 12pm to 01:30pm (GMT+2)
Paris / Berlin : Thursday, September 7th 2017 from 01pm to 02:30pm (GMT+2)
Istanbul : Thursday, September 7th 2017 from 02pm to 03:30pm (GMT+2)
Moscou / Dubaï : Thursday, September 7th 2017 from 03pm to 04:30pm (GMT+2)
Bangkok : Thursday, September 7th 2017 from 06pm to 07:30pm (GMT+2)
Shanghai : Thursday, September 7th 2017 from 07pm to 08:30pm (GMT+2)
Tokyo : Thursday, September 7th 2017 from 08pm to 09:30pm (GMT+2)
Sydney : Thursday, September 7th 2017 from 10pm to 11:30pm (GMT+2)
Wellington : Friday, September 8th 2017 from 12am to 01:30am (GMT+2)
San Francisco : Thursday, September 7th 2017 from 04am to 05:30am (GMT+2)
New York : Thursday, September 7th 2017 from 07am to 08:30am (GMT+2)
Buenos Aires : Thursday, September 7th 2017 from 08am to 09:30am (GMT+2)
Reykjavik : Thursday, September 7th 2017 from 11am to 12:30pm (GMT+2)
London / Dublin : Thursday, September 7th 2017 from 12pm to 01:30pm (GMT+2)
Paris / Berlin : Thursday, September 7th 2017 from 01pm to 02:30pm (GMT+2)
Istanbul : Thursday, September 7th 2017 from 02pm to 03:30pm (GMT+2)
Moscou / Dubaï : Thursday, September 7th 2017 from 03pm to 04:30pm (GMT+2)
Bangkok : Thursday, September 7th 2017 from 06pm to 07:30pm (GMT+2)
Shanghai : Thursday, September 7th 2017 from 07pm to 08:30pm (GMT+2)
Tokyo : Thursday, September 7th 2017 from 08pm to 09:30pm (GMT+2)
Sydney : Thursday, September 7th 2017 from 10pm to 11:30pm (GMT+2)
Wellington : Friday, September 8th 2017 from 12am to 01:30am (GMT+2)
The best choice in SFA procedures depending on multiple factors (Live Session)
Clinical - Anatomical - Cost efficiency
Share
Friday, June 29th 2018 from 09:40am to 11am (GMT+2)
Honolulu : Thursday, June 28th 2018 from 10:40pm to 12am (GMT+2)
San Francisco : Friday, June 29th 2018 from 01:40am to 03am (GMT+2)
New York : Friday, June 29th 2018 from 04:40am to 06am (GMT+2)
Buenos Aires : Friday, June 29th 2018 from 05:40am to 07am (GMT+2)
Reykjavik : Friday, June 29th 2018 from 08:40am to 10am (GMT+2)
London / Dublin : Friday, June 29th 2018 from 09:40am to 11am (GMT+2)
Paris / Berlin : Friday, June 29th 2018 from 10:40am to 12pm (GMT+2)
Istanbul : Friday, June 29th 2018 from 11:40am to 01pm (GMT+2)
Moscou / Dubaï : Friday, June 29th 2018 from 12:40pm to 02pm (GMT+2)
Bangkok : Friday, June 29th 2018 from 03:40pm to 05pm (GMT+2)
Shanghai : Friday, June 29th 2018 from 04:40pm to 06pm (GMT+2)
Tokyo : Friday, June 29th 2018 from 05:40pm to 07pm (GMT+2)
Sydney : Friday, June 29th 2018 from 07:40pm to 09pm (GMT+2)
Wellington : Friday, June 29th 2018 from 09:40pm to 11pm (GMT+2)
San Francisco : Friday, June 29th 2018 from 01:40am to 03am (GMT+2)
New York : Friday, June 29th 2018 from 04:40am to 06am (GMT+2)
Buenos Aires : Friday, June 29th 2018 from 05:40am to 07am (GMT+2)
Reykjavik : Friday, June 29th 2018 from 08:40am to 10am (GMT+2)
London / Dublin : Friday, June 29th 2018 from 09:40am to 11am (GMT+2)
Paris / Berlin : Friday, June 29th 2018 from 10:40am to 12pm (GMT+2)
Istanbul : Friday, June 29th 2018 from 11:40am to 01pm (GMT+2)
Moscou / Dubaï : Friday, June 29th 2018 from 12:40pm to 02pm (GMT+2)
Bangkok : Friday, June 29th 2018 from 03:40pm to 05pm (GMT+2)
Shanghai : Friday, June 29th 2018 from 04:40pm to 06pm (GMT+2)
Tokyo : Friday, June 29th 2018 from 05:40pm to 07pm (GMT+2)
Sydney : Friday, June 29th 2018 from 07:40pm to 09pm (GMT+2)
Wellington : Friday, June 29th 2018 from 09:40pm to 11pm (GMT+2)
Complex Right Coronary Artery CTO Procedure: Step-by-Step antegrade dissection reentry technique
Case of the month: September 2018 - Live Case #6 MLCTO 2018
Share
Provisional Bifurcation techniques to support bailout scenarios
Insights from the Visible Heart�...
Case of the month: July 2024
Share
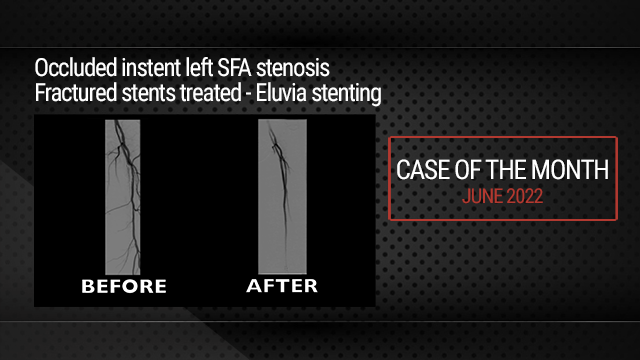
Occluded instent left SFA stenosis | Fractured stents treated - Eluvia stenting
Case of the month: June 2022
Share
Eluvia, designing a revolutionary drug eluting stent for SFA interventions
Lecture by Jaydeep Kokate
Share
TEVAR of the thoracic aneurysm with short neck below left common carotid artery using C TAG with act...
Case of the month: March 2022
Share





Alaaeldin H. what is the expected patency for this long segment ,multilevel occlusion.
Max A. Thank you for your comment. This patient requires a monthly follow up to maintain patency in order to assure ulcer healing . After 6 months the risk of restenosis and occlusion is high .
marcus P. Set good
Sandeep S. why did we have to break the end of Eluvia stent towards the end of deployment.
Georgi G. Leave a new comment to the discussion
Max A. It appears to be more convenient in long ELUVIA stent.
Collu B. Congratulations for very informative case