
Become an Incathlab member and receive full access to its content!
Registration Login
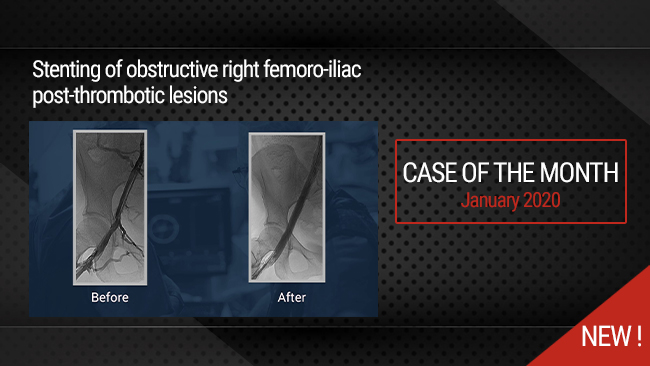
This case reports the use of the VICI stent to treat postthrombotic femoro-iliac obstructive lesions under IVUS guidance.
The patient had severe PTS, and required a previous contralateral lower limb amputation.
Educational objectives
- Technique of catheterism.
- Interest of the IVUS in lesions assessment including landing zones, stent length and diameter choice, and the final result.
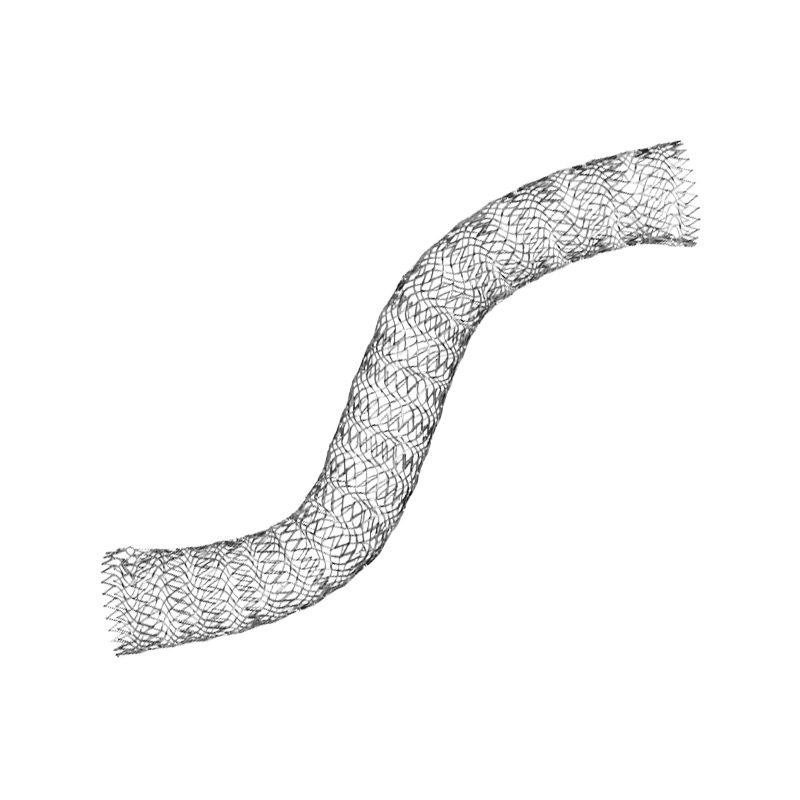
- Use of the VICI stent.
Step by step procedure
- Case introduction and MRV
This patient has a very severe clinical status with previous left limb amputation which is exceptional. MRV shows major right femoro-iliac vein obstructive lesions with a quite small common femoral vein and a good inflow from the deep femoral vein (femoral vein quite occluded).
- Access
Percutaneous femoral access was used in the severely diseased femoral vein but jugular access could also have been used.
- Catheterism
The common femoral and iliac veins are not occluded, so the lesions can be crossed quite easily with simple wire. It is mandatory to check on a profile view that the wire goes in front of the spine in order to check that it is into the IVC and not in collateral pathways.
- Material requirement
Predilatation must be performed using high pressure balloon and should be done at the diameter of the selected stent.
In venous stenting, large and long self-expanding stents must be used in order to avoid stent migration and to ensure a good flow into the treated segments (at least 6cm long and 14 to 16 mm in diameter)
- IVUS guidance
This exam depicts precisely the lesions and mostly the inflow and the landing zones. Indeed, phlebography by itself can be used but is far less precise than IVUS. While using phlebography only, proximal landing zone can be more accurately described by the inflation of a balloon into the femoro-iliac junction in order to precise the localization of the deep femoral vein.
In veins, it's very important to treat the lesions from one undiseased segment to another one, and not only to cover the lesions.
IVUS can also help to determine the diameter of the stent to be used even if in iliac veins it is recognized that 14 to 16mm stents must be always used.
- Stents deployment & Post-dilatation
The stents used in this case are Boston Scientific VICI stents. When multiple stents are used, an overlap of at least 2cm should always be performed to avoid the occurrence of an angulation between them.
The caudal end of the VICI stent shortens during deployment and post-dilatation so the operator should anticipate this phenomenon in order to avoid an insufficient coverage of the caudal landing zone. Another alternative with the VICI stent is to use the Verto which deploys reversely.
IVUS can be used after deployment of the first stent in order to assess the exact length needed to cover the whole lesions including the overlap.
Post-dilatation must be performed to ensure perfect stent deployment.
- Results assessment
Again, IVUS is the best way to evaluate the results and mainly the correct deployment of the stent that should have a circular aspect and should cover the landing zones while sparing confluences.
- Case summary, protocol & products used
Protocol
- Procedure time: 60 min
- Exposure time: 10 min
- Exposure: 74 mGray
- Contrast volume: 40 ml
Bibliography
Razavi MK, Black S, Gagne P, Chiacchierini R, Nicolini P, Marston W; VIRTUS Investigators. PivotalStudy of Endovenous Stent Placement for Symptomatic Iliofemoral Venous Obstruction. 2019 Dec 13.
Saleem T, Knight A, Raju S. Diagnostic yield of intravascular ultrasound in patients with clinical signs and symptoms of lower extremity venous disease. J Vasc Surg Venous Lymphat Disord. 2019 Oct 21.
Montminy ML, Thomasson JD, Tanaka GJ, Lamanilao LM, Crim W, Raju S. A comparison between intravascular ultrasound and venography in identifying key parameters essential for iliac vein stenting. J Vasc Surg Venous Lymphat Disord. 2019 Jun 10.
Last update : 2021-05-11
Our Cases of the Month
The case of the month is a new way for our users to watch, learn, and share with incathlab. They can watch a video that highlights an innovative case and uses excellent pedagogical techniques, lear...
Join the Discussion
Suggestions
San Francisco : Friday, June 29th 2018 from 12:40am to 02am (GMT+2)
New York : Friday, June 29th 2018 from 03:40am to 05am (GMT+2)
Buenos Aires : Friday, June 29th 2018 from 04:40am to 06am (GMT+2)
Reykjavik : Friday, June 29th 2018 from 07:40am to 09am (GMT+2)
London / Dublin : Friday, June 29th 2018 from 08:40am to 10am (GMT+2)
Paris / Berlin : Friday, June 29th 2018 from 09:40am to 11am (GMT+2)
Istanbul : Friday, June 29th 2018 from 10:40am to 12pm (GMT+2)
Moscou / Dubaï : Friday, June 29th 2018 from 11:40am to 01pm (GMT+2)
Bangkok : Friday, June 29th 2018 from 02:40pm to 04pm (GMT+2)
Shanghai : Friday, June 29th 2018 from 03:40pm to 05pm (GMT+2)
Tokyo : Friday, June 29th 2018 from 04:40pm to 06pm (GMT+2)
Sydney : Friday, June 29th 2018 from 06:40pm to 08pm (GMT+2)
Wellington : Friday, June 29th 2018 from 08:40pm to 10pm (GMT+2)




Rajesh K. do you regularly land the proximal end of the stent into IVC or try to land it at the confluence? If the external compression is at the confluence then would you be convinced to extend into IVC?
Mangesh T. 1. What was the "Hematological cause" for recurrent bilateral lower limb ilio-femoral DVT? What kind of Hypercoaguble state of the blood causing thrombosis?
2. Where is the Venous access & entry side (Mid-SFV in thigh) or CFV in groin?
3. How to fix up 10Fr large bore sheath in Chronically occluded femoral vein?
4.Venous inflow from Profunda femoris (Deep femoral) is Sufficient even if Common femoral is badly damaged?
5. Incase of "Infra-inguinal ligament" Venous stent extension and keeping it above lesser trochanter bony landmark for SFV-DFV Confluence zone; how much long term patency of 2 stents expected with post Stenting good oral Anticoagulation and Anti-Platelets??
Sameh S. highly educative