×
It looks like you're using an obsolete version of internet explorer. Internet explorer is no longer supported by Microsoft since the end of 2015. We invite you to use a newer browser such as Firefox, Google Chrome or Microsoft Edge.

Become an Incathlab member and receive full access to its content!
You must be an Incathlab member to access videos without any restrictions. Register for free in one minute and access all services provided by Incathlab.You will also be able to log into Incathlab from your Facebook or twitter account by clicking on login on the top-right corner of Incathlab website.
Registration Login
Registration Login
40850 views
Program
| 12.30 | Introduction |
| 12.32 |
Overview of devices: ○ Veniti stent – Stephen Black ○ Wallstent – Olivier Hartung ○ IVUS – Peter Neglen |
| 12.47 |
Case in box n°1: May-Thurner syndrome Panel discussion |
| 12.57 |
Case in box n°2: May-Thurner syndrome Panel discussion |
| 13.07 |
Acute DVT: ○ Goals and history of clot removal strategies – Yves Alimi ○ PMT - Stephen Black |
| 13.25 |
Treatment of chronic lesions: ○ Recanalization – Olivier Hartung |
| 13.33 |
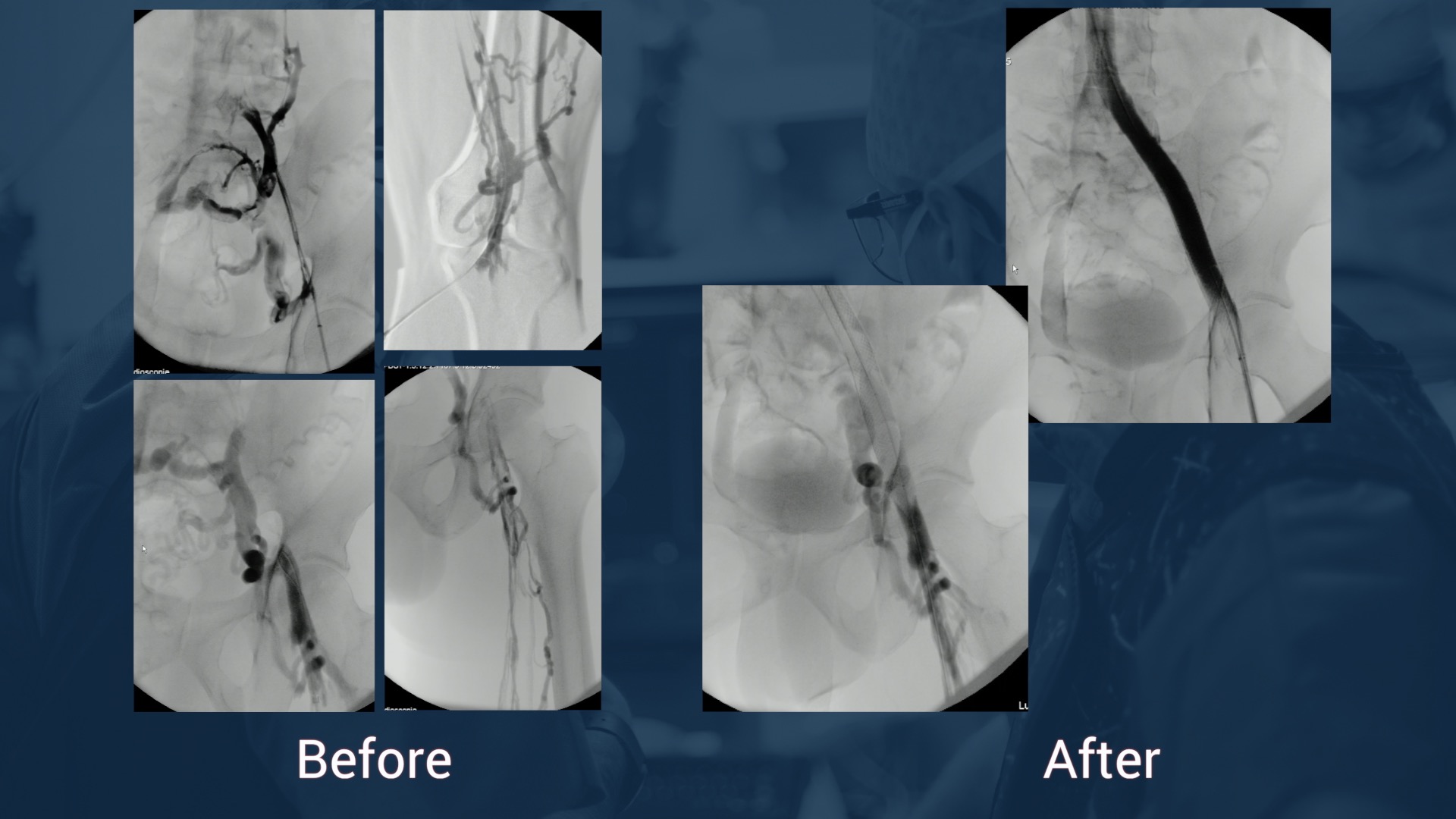
Case in box n°3: Left femoro iliac vein recanalization and stenting Panel discussion |
| 13.41 |
Case in box n°4: Left femoro iliac vein recanalization and stenting Panel discussion |
| 13.55 | Conclusion |
Educational objectives
- Diagnostic approach for patients with suspected ilio-femoral vein obstructions
-
Tips and Tricks for venous recanalization in patients with:
- Acute DVT
- May Thurner Syndrome
- Chronic obstructions of the ilio-femoral vein system
- Stent design, performance and available evidence
- Value of Intravascular ultrasound (IVUS) for venous recanalizsation
Audience
- Endovascular specialists (Vascular Surgeons, Interventional Radiologists, Angiologists and Interventional Cardiologists) interested and/or specialized in venous interventions
- Referring physicians of patients with venous disease
Shooting date : 2017-10-13
Last update : 2018-06-26
Last update : 2018-06-26
Join the Discussion
Suggestions
October 2016
Honolulu : Wednesday, October 19th 2016 from 01:30am to 03am (GMT+2)
San Francisco : Wednesday, October 19th 2016 from 04:30am to 06am (GMT+2)
New York : Wednesday, October 19th 2016 from 07:30am to 09am (GMT+2)
Buenos Aires : Wednesday, October 19th 2016 from 08:30am to 10am (GMT+2)
Reykjavik : Wednesday, October 19th 2016 from 11:30am to 01pm (GMT+2)
London / Dublin : Wednesday, October 19th 2016 from 12:30pm to 02pm (GMT+2)
Paris / Berlin : Wednesday, October 19th 2016 from 01:30pm to 03pm (GMT+2)
Istanbul : Wednesday, October 19th 2016 from 02:30pm to 04pm (GMT+2)
Moscou / Dubaï : Wednesday, October 19th 2016 from 03:30pm to 05pm (GMT+2)
Bangkok : Wednesday, October 19th 2016 from 06:30pm to 08pm (GMT+2)
Shanghai : Wednesday, October 19th 2016 from 07:30pm to 09pm (GMT+2)
Tokyo : Wednesday, October 19th 2016 from 08:30pm to 10pm (GMT+2)
Sydney : Wednesday, October 19th 2016 from 10:30pm to 12am (GMT+2)
Wellington : Thursday, October 20th 2016 from 12:30am to 02am (GMT+2)
San Francisco : Wednesday, October 19th 2016 from 04:30am to 06am (GMT+2)
New York : Wednesday, October 19th 2016 from 07:30am to 09am (GMT+2)
Buenos Aires : Wednesday, October 19th 2016 from 08:30am to 10am (GMT+2)
Reykjavik : Wednesday, October 19th 2016 from 11:30am to 01pm (GMT+2)
London / Dublin : Wednesday, October 19th 2016 from 12:30pm to 02pm (GMT+2)
Paris / Berlin : Wednesday, October 19th 2016 from 01:30pm to 03pm (GMT+2)
Istanbul : Wednesday, October 19th 2016 from 02:30pm to 04pm (GMT+2)
Moscou / Dubaï : Wednesday, October 19th 2016 from 03:30pm to 05pm (GMT+2)
Bangkok : Wednesday, October 19th 2016 from 06:30pm to 08pm (GMT+2)
Shanghai : Wednesday, October 19th 2016 from 07:30pm to 09pm (GMT+2)
Tokyo : Wednesday, October 19th 2016 from 08:30pm to 10pm (GMT+2)
Sydney : Wednesday, October 19th 2016 from 10:30pm to 12am (GMT+2)
Wellington : Thursday, October 20th 2016 from 12:30am to 02am (GMT+2)
Conquering complex femoropopliteal cases
New techniques and clinical evidences
Share
August 2013
Honolulu : Tuesday, August 27th 2013 from 05am to 07am (GMT+2)
San Francisco : Tuesday, August 27th 2013 from 08am to 10am (GMT+2)
New York : Tuesday, August 27th 2013 from 11am to 01pm (GMT+2)
Buenos Aires : Tuesday, August 27th 2013 from 12pm to 02pm (GMT+2)
Reykjavik : Tuesday, August 27th 2013 from 03pm to 05pm (GMT+2)
London / Dublin : Tuesday, August 27th 2013 from 04pm to 06pm (GMT+2)
Paris / Berlin : Tuesday, August 27th 2013 from 05pm to 07pm (GMT+2)
Istanbul : Tuesday, August 27th 2013 from 06pm to 08pm (GMT+2)
Moscou / Dubaï : Tuesday, August 27th 2013 from 07pm to 09pm (GMT+2)
Bangkok : Tuesday, August 27th 2013 from 10pm to 12am (GMT+2)
Shanghai : Tuesday, August 27th 2013 from 11pm to 01am (GMT+2)
Tokyo : Wednesday, August 28th 2013 from 12am to 02am (GMT+2)
Sydney : Wednesday, August 28th 2013 from 02am to 04am (GMT+2)
Wellington : Wednesday, August 28th 2013 from 04am to 06am (GMT+2)
San Francisco : Tuesday, August 27th 2013 from 08am to 10am (GMT+2)
New York : Tuesday, August 27th 2013 from 11am to 01pm (GMT+2)
Buenos Aires : Tuesday, August 27th 2013 from 12pm to 02pm (GMT+2)
Reykjavik : Tuesday, August 27th 2013 from 03pm to 05pm (GMT+2)
London / Dublin : Tuesday, August 27th 2013 from 04pm to 06pm (GMT+2)
Paris / Berlin : Tuesday, August 27th 2013 from 05pm to 07pm (GMT+2)
Istanbul : Tuesday, August 27th 2013 from 06pm to 08pm (GMT+2)
Moscou / Dubaï : Tuesday, August 27th 2013 from 07pm to 09pm (GMT+2)
Bangkok : Tuesday, August 27th 2013 from 10pm to 12am (GMT+2)
Shanghai : Tuesday, August 27th 2013 from 11pm to 01am (GMT+2)
Tokyo : Wednesday, August 28th 2013 from 12am to 02am (GMT+2)
Sydney : Wednesday, August 28th 2013 from 02am to 04am (GMT+2)
Wellington : Wednesday, August 28th 2013 from 04am to 06am (GMT+2)
Leipzig in Avignon: Update in femoro-popliteal recanalization
Live from Clinique Rhône-Durance, Avignon, France
Share
May 2012
Honolulu : Thursday, May 24th 2012 from 05:59am to 08:13am (GMT+2)
San Francisco : Thursday, May 24th 2012 from 08:59am to 11:13am (GMT+2)
New York : Thursday, May 24th 2012 from 11:59am to 02:13pm (GMT+2)
Buenos Aires : Thursday, May 24th 2012 from 12:59pm to 03:13pm (GMT+2)
Reykjavik : Thursday, May 24th 2012 from 03:59pm to 06:13pm (GMT+2)
London / Dublin : Thursday, May 24th 2012 from 04:59pm to 07:13pm (GMT+2)
Paris / Berlin : Thursday, May 24th 2012 from 05:59pm to 08:13pm (GMT+2)
Istanbul : Thursday, May 24th 2012 from 06:59pm to 09:13pm (GMT+2)
Moscou / Dubaï : Thursday, May 24th 2012 from 07:59pm to 10:13pm (GMT+2)
Bangkok : Thursday, May 24th 2012 from 10:59pm to 01:13am (GMT+2)
Shanghai : Thursday, May 24th 2012 from 11:59pm to 02:13am (GMT+2)
Tokyo : Friday, May 25th 2012 from 12:59am to 03:13am (GMT+2)
Sydney : Friday, May 25th 2012 from 02:59am to 05:13am (GMT+2)
Wellington : Friday, May 25th 2012 from 04:59am to 07:13am (GMT+2)
San Francisco : Thursday, May 24th 2012 from 08:59am to 11:13am (GMT+2)
New York : Thursday, May 24th 2012 from 11:59am to 02:13pm (GMT+2)
Buenos Aires : Thursday, May 24th 2012 from 12:59pm to 03:13pm (GMT+2)
Reykjavik : Thursday, May 24th 2012 from 03:59pm to 06:13pm (GMT+2)
London / Dublin : Thursday, May 24th 2012 from 04:59pm to 07:13pm (GMT+2)
Paris / Berlin : Thursday, May 24th 2012 from 05:59pm to 08:13pm (GMT+2)
Istanbul : Thursday, May 24th 2012 from 06:59pm to 09:13pm (GMT+2)
Moscou / Dubaï : Thursday, May 24th 2012 from 07:59pm to 10:13pm (GMT+2)
Bangkok : Thursday, May 24th 2012 from 10:59pm to 01:13am (GMT+2)
Shanghai : Thursday, May 24th 2012 from 11:59pm to 02:13am (GMT+2)
Tokyo : Friday, May 25th 2012 from 12:59am to 03:13am (GMT+2)
Sydney : Friday, May 25th 2012 from 02:59am to 05:13am (GMT+2)
Wellington : Friday, May 25th 2012 from 04:59am to 07:13am (GMT+2)
Discover the difference drug elution makes in the SFA with Zilver PTX stents:
Max Amor, Flavio Airoldi ,Peter Gaines, William Kai,Jorg Tessarek
Share
Attempt of recanalization with previous surgical thrombectomy
Dr Hartung & Dr Neglen - Decision of non-intervention after diagnostic
Share












Sharif Khashaba K. kindly improve the voice
Vanessa R. How do you treat venous non thrombotic in stent restenosis
Gustavo R. In chronic oclusion how often did you see instent stenosis in Iliocaval Wallstent
Olivier H. in our experience on 162 patients with a median follow-up of 44 months, primary patency is 70% at 60 months and assisted primary patency 85%
Peter N. Using the Wallstent, the cumulative in-stent stenosis rate at 6 years is in non-thrombotic obstructions (NIVL) 1% and in postthrombotic obstructions approximately 10%. In-stent stenosis is then defined as being >50% lumen reduction. It is common to see some in-stent layering of
Jacobo N. What do you think is the best aproach to the lesion, popliteal or contralateral? Thanks
Olivier H. for chronic lesion, i prefer anterograde approach through the femoral or popliteal. Some teams favor internal jugular approach (must always be ready in case of IVC lesions)
for acute lesions, it depends on the patency of the popliteal vein. If occluded, jugular or controlateral acess
Maria Fabrizia G. do you use the same strategy in presence of PE?
Olivier H. PE does not change the strategy but can make discuss the use of an IVC filter
bander A. what is he indications in case of non thrombotic iliac vein lesion ?
Olivier H. symptomatic and disabled patients C2-6, pelvic congestion syndrome
Peter N. I agree with Olivier, but wants to qualify it slightly. As we pointed out in the discussion, compression of the iliac veins are common in the asymptomatic population and possibly up to 30% have >50% stenosis with no symptoms! So there is a potential risk of overtreatment. In chronic venous disease of the lower limb, treatment of the outflow obstruction is indicated in patients with the C-class in CEAP being marked swelling (C3) and those with skin changes/ulcers (C4-C6). In addition, you have those patients with venous pain without skin changes or varicose veins, which can not be solely explained by the presence of reflux, if any. We use visual analogue scale (VAS) to evaluate that, considering VAS >5 being significant. As Olivier pointed out the symptoms have to affect the patients' quality of life.
Sandeep S. When using three stents, why is the middle stent placed last in iliofemoral venous intervention?
Is there any algorithim to decide on when and not to stent across deep femoral vein?