
Devenez membre d'Incathlab et bénéficiez d'un accès complet !
Inscription Connexion
Learning objectives
- To share knowledge and experience about OCT and FFR solutions to improve patients outcome in complex lesions
- To demonstrate ease of use of performing FFR and OCT in daily practice using a fully integrated solution
- To better understand to whom, when and how to use OCT and FFR through a review of the latest clinical evidence
Moderator
Dr. Jonathan Byrne | King's College Hospital, UK
Program
First PCI Optimization Recorded Case
Acute coronary Syndrome with inferolateral Ischemia :
PCI guided by FFR & angio co-registered OCT
By Dr. Jonathan M Hill | King's College Hospital, UK
Lecture : The Value of FFR in the Real World for Stable and Acute Patients
Dr. Narbeh Melikian | King's College Hospital, UK
Second PCI Optimization Recorded Case
Revascularisation prior to TAVI :
How an angio co-registered OCT provides
guidance for treatment
By Dr. Jonathan M Hill | King's College Hospital, UK
Is Angio Enough to Make a Good Decision in ACS?
Dr. Jonathan M Hill | King's College Hospital, UK
Questions and Discussion
Live session produced in collaboration with

One addtionnal recorded cases on the same subject:
OCT and Angio coregistration for stent optimisation in surgical turndown
Dernière mise à jour : 09/06/2021
OPTIS™ Integrated System / St. Jude Medical
The power of integration: Innovative solutions to optimize PCI in daily practice
(From King's College Hospital)
Operators
- Dr. Jonathan Hill | London, UK | Cardiologist
- Dr. Jonathan Byrne | London, UK | Cardiologist
- Dr. Narbeh Melikian | London, UK | Cardiologist
Moderator
- Dr. Jonathan Byrne | King's College Hospital, UK
Dr. Jonathan Hill:
Welcome to King’s College Hospital. My name is Jonathan Hill. I’m one of the consultant interventional cardiologists here at King’s. King’s is a busy hospital in South London. We’re an acute cardiac centre. We are a very active interventional centre with a big cardiac surgery program as well. And we have a variety of complex cases.
What we’re going to be talking about today is the power of integration—looking at innovative solutions to optimize PCI in daily practice.
The objectives of the meeting today for this webinar are:
- To share our insights and knowledge about OCT and FFR, and look at improving patient’s outcome in some of the complex cases
- What we want to do is to demonstrate the ease of use when performing FFR and OCT in daily practice. We’re going to be looking at a new piece of technology which allows us to completely integrate angiography with OCT. This is a system which is always ready and always on in the cath lab.
- We want to better understand in our patients when and how to use OCT and FFR through a number of clinical cases. We’ve got three clinical cases that we’re going to present, and I’ve got some presentations as well of clinical data.
First PCI Optimization Recorded Case
Dr. Jonathan Hill:
Let’s get on with the first case. While we’re doing this presentation, I just want to remind you that we’re able to ask questions through the web chat forum. So please, if you’ve got questions, please ask them as we go along. We’ll attempt to address these questions somewhere during the course of this webinar.
This is the first case. It’s a 67 year-old male. It’s a very typical patient for us here at King’s. He’s had previous myocardial infarction. He presented to a clinic very recently in the last 48 hours. And he has a background of previous over the course of the last 10 years with angioplasty, with stent implantation to the left anterior descending artery, the right coronary artery, and a distal branch of the right coronary in the posterolateral territory. He presented in an outpatient setting, but in fact was quite unwell with that presentation, with symptoms at rest. He developed rest pain on the morning of the clinic and came to clinic in the afternoon. ECG had showed widespread inferolateral ischaemia. So this is a patient presenting with a background of significant coronary disease with what looks like a high-risk acute coronary syndrome. The patient was duly admitted with an immediate treatment plan for further investigation with urgent angiography.
Let’s move on to the case.
Acute coronary Syndrome with inferolateral Ischaemia:
PCI guided by FFR & angio co-registered OCT
By Dr. Jonathan M Hill | King's College Hospital, UK
Dr. Jonathan Hill:
We’re just going through the coronary angiogram here. This gentleman has presented with suspected acute coronary syndrome. He’s had chest pain at rest on a background of previous intervention. We can see from this initial angiographic shot that he’s had intervention in the LAD. You can see that segment of fairly dense stent struts evident there. And there is an apparent stenosis at the origin of a fairly sizable diagonal, which is adjacent to that LAD. We can see within the right, possibly in the PDA or posterolateral branch, there’s a stent which is large calibre in its proximal segment.
Going on to the next image, in the LAO cranial, you can appreciate that there is the stent within the LAD. You can see the stenosis at the origin of that diagonal vessel. I can’t see any stent thrombosis, but there is a degree of irregularity within the LAD stented segment. If you see in the AV circumflex, you can see in that vessel, just on the horizon there (on the top right of the picture), that there is a stenosis within that vessel. That maybe something that requires further interrogation.
Next view. This is in the PA cranial—10°-40° RAO cranial, in fact. You can see those two diagonals: one of them before the stent, one of them adjacent to the stent. That’s possibly something that was in that state at the end of that intervention, or that may be restenosis which has occurred more recently.
Next shot. I can’t really see a potential acute lesion, possibly within that circumflex system. We may come back to that.
Next. Again, you can see within that circumflex system, but again it doesn’t appear to be angiographically significant. We may come in and interpret that with either an FFR, OCT, or possibly both.
Next, moving on to the right coronary artery. This is really quite a heavily dominant vessel as you can see. And I think working our way down through various segments—In the proximal segment, you can see that degree of irregularity. You can see that there is a degree of haziness in the proximal segment. You can see a stented segment, and that segment looks absolutely fine. And the distal third, proximal to the crux there, also looks good.
Go to the next view. Opening up the PDA, two posterolateral ventricular branches. At the middle of those branches, there looks to be a significant stenosis, angiographically at least, in that vessel—quite a long vessel but quite small in calibre.
Next. This is the PA cranial projection. And you can appreciate that the stented segment in that very distal large PLV system looks good. And possibly something in the origin of that middle PLV branch. The PDA itself looks good. Again, you can see that stenosis in the proximal segment of the right coronary artery, and I’d like to get some more information about that.
Next. The point we’re at now is we have the pressure wire ready to go. We’ve used the integrated system here, so it’s fairly easy to setup. We’ve used the table side controller. We’re just pressing ‘P’ until we’re ready to go. We’ve now equalized. I’m just going to put the wire down through this stented segment. We’re just being careful to pull out the needle and equalize again. Using the table side controller, click on equalize. And now we’re ready to go.
I find the Aeris wire quite easy to manipulate in comparison to the fixed-wire system. We’re going to go through the stent. I’m going to position this tip within the PDA. We’re going down the PDA, trying to get that beyond the crux. This is really just to assess in isolation the proximal segment rather than that distal lesion. We can start now.
Even at rest, I’m not particularly convinced that this is going to be significant. I’ve ordered a dose of 140 mcg/kg/min. Press P to start recording. Thank you. I’m going to pull back now to show you where we are. Looking at the angiogram, I’m coming proximal to the segment of the stent. That’s the hazy lesion, and that’s the step-up point. So it’s now back to normal. And stop. We will equalize again, just to make sure we’re correcting for any drift. Re-equalized.
This time I’m going to go into the PLV. Having the table side controller makes it much easy to do all these equalization manoeuvres. This would be a role normally taken by the physiologist within the lab. I think this just streamlines the workflow a little. You can see it is a pretty long vessel. That’s just confirming its position. You can see it’s quite an easily manoeuvrable wire. Values settled again—not a significant pressure difference at rest. Can we increase the dose please to 175mcg/kg/min? Yeah, off we go.
I’m going to start now. Just press ‘P’. You can see the effects already. Suddenly, angiographically, this lesion looks significant to me. Stop. The wire is down. I’m now going to do an OCT study. I’m now going to look at those two areas of plaque: one within the origin of the PLV, and the other within the proximal segment of the right coronary artery.
This gentleman has presented with symptoms at rest. We can now see some changes in the lateral leads, or anterolateral leads. Whether that’s attributable to that large distal posterolateral circumflex… or possibly is that more of diagonal-related artery? Well, maybe it’s caused by the origin of that second diagonal that we saw on the left coronary pictures. Let’s get some more information about the plaque within this vessel. Hopefully we can just get into the origin there.
Let’s look at this first segment. Auto-calibrate. Press now. Now we’ve got both the OCT and the angiogram recorded at the same time. What we’re going to be interpreting is that segment. From the imaging catheter, you can see it moving back on that image. And what the opticized system allows us to do is to then track that catheter. And each of those points within that vessel is co-registered with the angiogram and the OCT image. We’re now going to click co-register. I’ve got to identify the vessel of interest, which is here. That’s actually near where the laser-imaging catheter is. Here. And then we’re going to move proximal, which is here. That’s the segment that we’re interpreting. Let’s see if this will try and do it. Okay, so that has worked.
I’m going to move down. What I want to do now is to move to that segment which caught my eye. I’m rotating the bedside controller—table side controller. You can see, I’ve now move into that segment. That’s really where it looked very hazy. And in fact, I can see that there is a lesion on the longitudinal view. And if you look at the axial view—that’s the top right here—there is a significant circumferential plaque there. You can see that there is probably some fibrous plaque. This is non-calcified. I’m looking for a thin-capped fibroatheroma. You can probably see. I think there’s a lipid pool there. You can see this area between around 7 and 10 o’clock, which I think is a lipid pool in this area of haziness within the origin of that PLV.
We’re going to do some measurements. One of the measurements I like doing is bringing up the lumen profile. Make sure properly… accept that. What this is going to do is it gives you the mean luminal diameter and the areas from the distal vessel. In fact, I can see, even though it’s quite a small vessel, in this segment—this is pressure wire negative. Clearly, at this point, the MLA is 1.29 mm2. Is that a significant lesion? Well, it’s not significant angiographically. But perhaps if we look at this area in a bit more detail, there’s definitely plaque. Here you can see fairly significant plaque from an OCT perspective, and there’s fibroatheroma, with some lipid pool there. Is there any plaque rupture? Plaque erosion? Or maybe you can in this area here, possibly here, there’s some plaque disruption on the surface of that. Maybe that’s sufficient reason for this gentleman to have had pain which has now subsided.
We’ll do a new recording. We can come back to those readings. We’re going to position this catheter now, and we can just image… Move the table over please so I can see the angiogram. That’s it. We’re going to look at this segment here. This will give us a view through the stent and that proximal segment. You can see on the coronary angiogram the tip of the imaging component—the catheter moving back through the stented segment. These are nice, clear pictures. Let’s go and co-register them. That’s fine. Distal to proximal. Confirm. And now we’re just waiting for the co-registration to happen. That line looks right, so we’ll accept that.
Let’s come to that—the angiogram. Let’s rotate up to that area which I was concerned about, looking a bit… that’s within the stent. It was this bit here. Oh, it’s moving off. Move back on. In fact, that’s that hazy area. In fact, there’s the plaque that’s possibly plaque rupture. Certainly, this is a very suspicious area within the artery. I’m coming back out to a nice calibre. I can see little bit of something there in the vessel. Is that thrombus? No, possibly not.
Let’s put lumen profile on again. You need to calibrate before you do that. Let’s accept that. What I’m interested in is what the lumen profile is. Anything under 4mm2… there we go—3.48mm2. Now, we know that that’s physiologically insignificant. But this gentleman is presenting in the context of an acute coronary syndrome. He’s got a highly suspicious looking plaque in this segment with endothelial disruption. In fact, this segment here is something that I’m drawn to on the OCT. Certainly your eyes were drawn to it on the angiogram, but I think it’s something that’s potentially treatable. I’m not concerned about the stent. I’m going to set my distal marker. We’ll look around the stent. Certainly, in this segment, there is an area of stenosis proximal or in the run into the stent. I’m looking at the stent length here of around 24mm, and I’m going to bring it into the proximal end of this stent across this lesion. I’m just looking at the diameter of this vessel. I’m just going to make a measurement—a simple measurement of this vessel. That’s 4.2mm. That’s 3.9mm. And the luminal diameter here is around 3.5mm. Certainly, a 3.5mm stent in this segment would be apposed. Okay. Let’s take this out. Yeah. We can give some more of that. That would be good.
Can I have a stent please? Okay. Can I just have a 2T5x12mm please? Okay. Let’s go to this area.
Okay, that’s fine. Very nice.
Okay. Let’s come to the LAO cranial view—LAO 20°. We’re now going to position the stent in the origin of the PLV. Give me a little injection. Down again. And up again. Flatter 3.5x24mm please? I think that looks well deployed. We could come back and have a look with OCT, but we’ve made our measurements from the OCT fairly accurately. 3.5mm, please.
This is the hazy area. If we move down, that’s exactly where we’re heading for. That hazy area here corresponds to that plaque rupture we see in that proximal vessel. Again, if you could give me a little tester injection. We’re now positioning the stent, definitely covering that lesion, I hope. The outer diameter at 20 is 4.15mm. This is a stent which should, in theory, because of its architecture, heal relatively rapidly, and by rapidly I mean within the first few months of implantation. Now we really do have a genuine prospect of reducing antiplatelet therapy down definitely to 3 months, but possibly even down to as low as 1 month.
We’re going to do a study now of the stent to confirm apposition. We should get the distal end of the original stent and the proximal end of the new stent. Okay. Looks like we have good clearance. We have not quite got the proximal edge there. Let’s just check if we… Let’s come to the edge. I need to see the edge. All right. We’re fine. So, let’s co-register. Continue. Confirm. Now the co-registration is happening. It looks fine. Just coming in, I can see the stent struts cut obliquely here. That’s the edge. You can see them embedded. They are embedded. There isn’t much material extruding through. That’s the side branch you see, with the strut across it. And you can see on the axial views here, we’ll mark this up. Let’s come down. That’s all looking really well-apposed. That’s the area where we’ve now stented this plaque. This is all perfectly deployed. No areas of mal-apposition. You can see the stent architecture here, and you can see it is quite a big cell design. Here you can see the interconnects between the stents. I think in this design there’s two interconnects. And we head then down to the old stented segment. This is the covered stent—the struts are covered, I mean. Then we’ll come back up, and this is the point you see on the 3D where the struts are heading into that region here. That’s the point where the new stent starts. And it all looks, by OCT at least, well-deployed. We’ll take the OCT catheter out.
Come in to the PA cranial please. Can I have nitrate? You can see the lesion in the middle PLV branch. Looks good. No significant stenosis. Then we’ll come over to the 20-20 view. I’ll take the wire out. We’ve treated the area of plaque rupture in the proximal vessel. That all looks very nice. Come back to the RAO. Take a final shot there. Sorry, LAO, I mean. Okay. Great. Flow looks good. Angiography looks good. OCT confirms it. It all looks fine as well.
Discussion
Dr. Jonathan Byrne:
Thank you very much, Jonathan. That was a very beautiful case with some fascinating new technology. If we can go back to the beginning, there’s some several very important and interesting areas we should cover in this case.
First of all, this man is presenting acutely. You very beautifully demonstrated the limitations of physiology in somebody presenting with an acute coronary syndrome with plaque rupture. Your FFR was negative, and it shows that really we are dependent on angiography anatomy and history in this situation. Perhaps you could comment further on which of the technology you believe and why you believe in this situation.
Dr. Jonathan Hill:
I suppose it’s not necessarily what I believe but about what we’re looking at pathologically. In a patient who’s coming in with a potential plaque rupture which is the pathological feature, changes in physiology in distal perfusion may not be relevant to treating that pathology. If you’re going to treat the lesion because it’s ruptured, then that’s what the procedure is being done for. It’s not to change the physiology. It’s to change the possibility of a further plaque event or further vessel occlusion. I think that’s what we’re treating. We are passivating plaque which is misbehaving rather than treating a distal perfusion problem created by a fixed stenosis. We’re dealing with a dynamic process within the vessel walls. That’s what we’re treating. And we can’t recognize that process with a pressure wire. We may, in some situations—it may well be pressure wire positive, physiologically positive. But I think this particular case, it’s a case that we all see fairly frequently. It’s somebody who presents with apparent ischaemia on an ECG. This gentleman had inferolateral ischaemia. We saw him initially with chest pain. And by the time he came to the cath lab, as is often the case, the chest pain had settled down. His ECG wasn’t quite so severe in terms of the ischemic changes. So we’re then faced with somebody whom you’ve shown is physiologically ischemic at rest, comes to the cath lab, and it doesn’t appear to be ischemic by pressure wire. But the pathology is still there.
Dr. Jonathan Byrne:
I think it’s the question of reliability of the pressure wire assessment in the setting of plaque rupture and the effects on the microvasculature. I think it’s very important that we use the techniques that are relevant in our setting. Certainly, anatomy is very useful. You’ve beautifully showed two areas of concern, possible plaque rupture. And one of the questions that has been asked—I think it’s fairly relevant to ask—is how often do you think this form of co-registration should be used or could be used in our day-to-day practice?
Dr. Jonathan Hill:
We’re looking for a tool that helps us make a better decision on the basis of an angiogram. When we’re doing FFR, we’re doing it because we accept that the angiogram is not sufficient to help us make the decision on the basis of some physiological parameter that we’re trying to treat. If you apply that same principle that angiography is insufficient to make the diagnosis, then in the acute coronary syndrome, I think the same principle applies. What OCT does here is it makes your angiography better. It’s a tool that when you fuse them together… You’d say, “When I look at this artery with this segment that looks a bit hazy angiographically, if I can then go to a high-resolution form of imaging,” and say, “Well, I want to know more information about this lesion…” If as an experience interventionist, you’re saying, “Well, I’m a bit suspicious about this,” and that’s how we would make the decision in the past, angiographically. You’d put a stent in because you’ve the seen patient presented with ischaemia and ECG changes. What OCT does is it takes away that uncertainty. It shows the pathology happening in front of your eyes.
Dr. Jonathan Byrne:
And one great question is how often do we use it? How often do you use it in day-to-day practice? What volume do you use on a daily basis?
Dr. Jonathan Hill:
Well, we’re a centre. We’re doing our physiologically-driven intervention around 1500-1600 cases a year, maybe 400-500 pressure wire studies, and around 200+ OCT studies. A significant proportion of our cases have physiological guidance and also anatomical guidance. What I think this will do is when we’re using OCT in these cases, and perhaps there’s an indication for more widespread use, in perhaps maybe 1 in 3 or 1 in 4 cases, I think it adds something to your diagnostic decision-making. We’re exploring this technology now. It’s a relatively new piece of technology of being able to register an angiogram with an OCT. I think it’s the first OCT system that’s able to do that. I think there are systems now being installed around the world. You know, this is one of the first systems in the UK. I think what we have to do is to use the tool, and I think we have to learn about pathology using this tool. I think it’s going to be used quite frequently.
Dr. Jonathan Byrne:
Absolutely. Now there’s some great questions coming through on the practicalities of the case and how adenosine was administered, whether centrally or peripherally. And although many of these will be answered in Dr. Melikian’s talk which is next, there are a couple of specific points I’d like to make. One of the questions is, “How is adenosine given?” Traditionally, certainly in the early studies, there’s a suggestion that you could only achieve hyperaemia from the femoral approach. We’ve recently published on adenosine given peripherally via our hand vein, showing that it gives identical amounts of hyperaemia. We use our hand or antecubital fossa infusion for adenosine. We use either the low or the high rate depending on the lab, but the low rate’s often used. And essentially, that’s how we do the procedures. I think a lot of the other FFR-related questions will be answered in the next talk. I think we should probably leave them to Dr. Melikian. Thank you very much for such an elegant demonstration of a day-to-day coronary case.
Dr. Jonathan Hill:
Thanks!
Dr. Jonathan Byrne:
Now I’m going to move on to Dr. Melikian’s lecture.
Lecture: The Value of FFR in the Real World for Stable and Acute Patients
Dr. Narbeh Melikian | King's College Hospital, UK
Dr. Narbeh Melikian:
Good afternoon ladies and gentlemen, and welcome to King’s. My name is Narbeh Melikian, and I’m one of the interventional cardiologists here at King’s College Hospital, and I’m senior lecturer in cardiology at King’s College London School of Medicine. Over the next 15 minutes or so, I would like to briefly tell you about what my views are about the use of FFR in the real world, and also, make specific reference to the role of FFR in patients with stable coronary disease and its use in acute coronary syndromes.
I’d like to start off by perhaps stating the obvious that even in 2015, angiography remains the gold standard for imaging coronary vessels. Although we have come a long way from when mavericks such as Werner Forssmann or Mason Sones conducted angiography, the main problems with coronary angiography remain the same, namely, that the angiogram is a two-dimensional representation of a three-dimensional structure, the coronary artery. As such, it can be extremely deceptive.
Over the years, there has been a wealth of data, as you can see in this slide, starting from fairly old trials, and moving into the modern era with COURAGE and the FAME series of trials, which have demonstrated that cardiac prognosis is primarily dependent on the presence of myocardial ischaemia and not the extent of epicardial vessel stenosis. So function is very important. And this is particularly relevant in vessels with intermediate angiographic disease—not ones where the arteries look smooth or have minor atheroma, and not vessels at the other end of the spectrum where we have significant stenosis, but the vast majority of patients who fall in between the two ends of the spectrum.
The question therefore becomes, “What is the optimal modality to detect myocardial ischaemia?” Do we use exercise treadmill test? Old fashioned tests? Do we use tests such as myocardial perfusion imaging, or stress echocardiography, or stress MRI? Imaging modalities which are very high on technology? Do we use intra-coronary imaging techniques such as OCT or intravascular ultrasound? Or do we use intracoronary physiology? I’m sure there are lots of people around the world who still, like this gentleman that I put on the screen, just stents everything that they see.
Now I would like to argue over the next few minutes that, in my opinion, the FFR (fractional flow reserve) is really the gold standard index that we should be using. It’s easily obtainable by measuring the pressure distal to a stenosis (PD) and comparing that to the pressure proximal to a stenosis. The ratio of the two derives FFR. Now, why do I think it’s the gold standard? There’s trial data—there’s a lot of trial data that we can talk to, but I’d like to just refer to two studies which summarize the essence of what FFR is all about in real world practice. This is the FAME series of trials. FAME I, which is what it’s now known, was a comparison of angiographic-guided PCI with FFR-guided PCI in patients with multi-vessel disease. We can see from this Kaplan-Meier curve, which is a summary of this very large trial published in the New England Journal of Medicine, that patients who underwent FFR-guided PCI at one year, and now we know longer, had a better outcome than individuals who had angiography-guided PCI.
And then came FAME II, which extended this information. Patients with physiologically significant stenosis were then randomized essentially to optimal medical therapy and intervention or just optimal medical therapy on its own. The slide on the right hand side of the screen essentially summarizes the results in that patients who were randomized to optimal medical therapy with a physiologically significant stenosis had greater number of events at 12 months than individuals who had angioplasty alone. This was driven primarily by the need for repeat revascularization.
Supplementing this trial evidence is a whole host of real-world registry experience which we now have. The Aalst Registry, the RIPCORD registry, the Mayo Clinic registry, and there are others from different countries which have been published. These registries incorporate the outcome of patients who have had FFR-guided intervention over a number of years, and some of them have many hundreds of thousands of patients in them.
Moving on from the trial evidence, why is FFR suitable in clinical practice? In my view, there are a number of very important and simple reasons why FFR is superior to other physiological indices from a practical point of view. First of all, it’s diagnostically accurate in multi-vessel disease. It has very high spatial resolution. It is highly reproducible and the results are not open to interpretation. It’s available in the catheter laboratory, so we can make measurements at the same time as the invasive studies. And finally, it could also be used to measure other physiological indices such IMR (index of myocardial resistance) to look at microvascular function.
Let’s address each one of these points one by one.
Diagnostically accurate in multi-vessel disease
I want to illustrate this by demonstrating a case—a simple case—67-year-old male gentleman with intermittent chest discomfort and some risk factors. The patient underwent a myocardial perfusion scan which demonstrated reduced perfusion in the circumflex territory. The cartoon of the angiogram that you could see demonstrates at least two-vessel disease in the right coronary artery and in the circumflex artery. So we have perfusion imaging which indicates patient has one-vessel disease, and angiography which indicates the patient has two-vessel disease. If we were to use the current evidence that physiology should determine intervention, then this patient should undergo revascularization in the circumflex territory. The person who was looking after this individual felt that it was slightly unusual that the very tight stenosis in the right coronary artery was not significant on the myocardial perfusion imaging, and the patient underwent multi-vessel FFR assessment. As you can see, all three vessels had a significant FFR. Hence, what we have is a patient with 3-vessel disease—so the moderate stenosis in the LAD is also positive here—who should potentially, according to current guidelines, probably have coronary artery bypass graft surgery.
FFR does not suffer from a major limitation of perfusion imaging techniques which is balanced ischaemia. We have looked at this by comparing FFR with myocardial perfusion imaging. We found that in comparison to FFR, perfusion imaging had a very low sensitivity and specificity in patients with multivessel coronary disease.
High Spatial Resolution
Let’s have a look at this case. The angiogram here demonstrates, as you can see, disease in the LAD and diagonal artery. However, the functional tests, for example the myocardial perfusion imaging, demonstrates ischaemia in the LAD territory; and the stress echocardiogram, if you look at the maximal workload here on the right hand bottom corner, demonstrates evidence of ischaemia again in the left anterior descending territory. However, FFR interrogation of these arteries gives us a very different view in that both the diagonal and the left anterior descending are positive. This is quite important in that no other functional modality has the same resolution as FFR. Exercise testing—the resolution is confined to the entire myocardium. Stress echocardiography—the resolution is confined to the level of epicardial vessel territory, as is magnetic resonance imaging techniques. Perfusion imaging, including PET, has exactly the same extent of resolution. However, the resolution in FFR is the length of the transducer at the tip of the wire which is a millimetre or so. So we can have per millimetre analysis of physiology in arteries with FFR which is not possible with any other modality of functional testing
Not Open to Interpretation
FFR is not open to different interpretation. Here are two stress echocardiograms from different patients, both of whom have significant LAD disease. It is easy in Patient A to see that there is evidence of hyperkinesia at maximal stress at the level of the apex, but this is not easily identifiable in Patient B. There is a significant inter-observer and intra-observer differential in reporting of stress techniques both in MRI as well as with echocardiography. FFR is not open to this bias, and is, in that sense, really unique as far as functional testing is concerned.
Highly Reproducible and Not Influenced by Haemodynamic Parameters
The results are highly reproducible. If we measure it in the same stenosis in sequence, we could see that the FFR value obtained is the same. And haemodynamic data, for example contractility, heart rate, and blood pressure, do not affect the actual results with fractional flow reserve.
Available in the catheter laboratory
Finally, a very simple issue is that it is available in the cardiac catheter laboratory. We are undertaking angiography which gives us anatomical information, and the FFR gives us the physiological information. So in the same place, at the same time, we can make a decision. There’s no requirement to take the patient off the cardiac catheter table to another part of the hospital on a different day for them to undergo a different modality of test, and then, if positive, for them to return to the cardiac catheter laboratory for an intervention. So it is very efficient from a time point of view as well as from a financial point of view. And in these days where finances can be tight in most healthcare systems, this is an extremely important point. Analysis of a trial data, for example FAME, have also shown that FFR-guided intervention is much more cost-effective than angiography-guided intervention.
Can be used assess other physiological indices
As I alluded to earlier on, we can use other physiological indices—some of these are for research, others can give us information about the viability of the microcirculation in the patient such as the index of myocardial resistance.
But like everything else, there are pitfalls with FFR. FFR is not by any means perfect, although, in my view, much better than other indices and techniques that we could use. We should be careful when assessing ostial stenoses, patients with acute coronary syndrome—it’s a major limitation of FFR—vessels with serial stenosis, and also in patients who have ventricular hypertrophy.
In this regard, I would to talk a little bit about patients with acute coronary syndrome because they constitute a large proportion of patients who pass through cardiac catheter laboratories. I have summarized the situation as to where, on the basis of current evidence, we can confidently use FFR, and where we should be cautioned, and what are the scenario where FFR should not be used. Let’s start with the latter comment that I made. FFR cannot be used in the acute phase of a patient suffering an ST-elevation myocardial infarction. However, FFR is perfectly reproducible and is entirely acceptable to use it both in the acute and non-acute phase in non-culprit vessels. How about the culprit vessel in the non-acute phase? That essentially are patients who’ve had a non-ST elevation infarction. There is emerging evidence from a number of studies which have been carried out that potentially in a group of patients this could be used, but it is entirely dependent on the viability of the microcirculation in that territory. This is where other physiological indices such as IMR may be of value or other anatomical values, for example interrogation of the lesion using intravascular ultrasound or with optical coherence tomography (OCT). I’d like to point out, therefore, that FFR-derived physiological data is only one of a number of pieces of information that we should use in the cardiac catheter laboratory to determine treatment for a particular patient. And the information is complementary to the anatomical data that is derived from OCT or IVUS. It should not be used instead of but in addition to that information. I’m sure the future really is dependent on the use of both physiological and anatomical data concurrently in a cardiac catheter laboratory to determine the optimal treatment modality for a patient.
Thank you very much for your attention.
Discussion
Dr. Jonathan Byrne:
Thank you very much, Narbeh, for that elegant presentation. It has answered many of the questions that are coming through. Perhaps I could ask you one or two simple procedural questions which are very high in the agenda for many of our audience. You talked about FFR and the protocol for FFR. Perhaps you could talk me through when or if you use intravenous vs. bolus doses of adenosine.
Dr. Narbeh Melikian:
In general, I tend to use intravenous all the time. I think you alluded to the fact that we also have recently published on the use of intravenous infusion of adenosine via a peripheral large antecubital vein. Primarily I use intravenous because it also gives the luxury of doing a pull-back if necessary. However, it’s not that I never use bolus intracoronary adenosine. These are primarily used for assessing Type A or simple single lesions in a straightforward case. So, the simple answer is, the default position is intravenous, but I do also occasionally use intracoronary.
Dr. Jonathan Byrne:
Sure. One of the situations you mentioned which is always difficult is that of serial stenosis within the vessel. How would you assess and treat serial lesions within a single vessel?
Dr. Narbeh Melikian:
One of the limitations of using FFR is in serial stenosis. Before I even embark on using FFR to determine which one of the two stenoses is important, the decision I make is whether both lesions could be treated percutaneously or not. When we do a pull-back, the conventional wisdom is that the greatest step-up in FFR or change in pressure should be treated first. And then FFR should be measured again across the remaining stenosis. Now, it may be that once the original stenosis has been treated, the second remaining stenosis also becomes then positive. These are determined by the complex laws of fluid dynamics. If the repeat measurement indicates that it is positive, we have to be prepared to treat that lesion as well. So I start off by initially determining anatomically that both could be treated, I measure FFR across both during pull-back, treat the greatest step-up, and then repeat FFR again. Depending on the result, I either leave the remaining stenosis if it’s negative, or if it’s positive, then that is also treated.
Dr. Jonathan Byrne:
Thank you. And the other important question we’ve touched almost in the first case is the utility of FFR in acute coronary syndromes. In first case, very elegantly demonstrated are two potential areas of plaque rupture. The utility of FFR in that setting is certainly questionable. Are there any situations where you would use FFR in an acute non-occluded vessel in acute coronary syndrome?
Dr. Narbeh Melikian:
Again, this is a scenario of controversy. There’s a huge amount of discussion around this topic at the moment. The main limitation for using FFR in the context of acute coronary syndrome is that the microcirculation in that vessel—the physiological function of the microcirculation—maybe disrupted. The problem is that the rate of recovery can vary between different patients. When measuring FFR, we have always got to remember that. If the FFR is positive, then it has answered that question. But if it’s negative, then it maybe a false negative. And the clinical picture and adjunct intra-coronary imaging techniques maybe of value to determine whether the individual needs to be treated or not. It’s also worthwhile remembering that there are occasions where, in the context of acute coronary syndrome, we may want to treat the artery not necessarily because the FFR is positive but because the anatomy dictates that it ought to be treated—for example, in a dissected vessel, or when there is acute plaque rupture. This is in itself, as I’m sure you know, is an area of great debate: whether stenting an acute ulcerated plaque is appropriate or whether it’s not appropriate.
Dr. Jonathan Byrne:
Thank you. It’s certainly a controversial area. I think on that note, perhaps we should move to the second recorded case.
Second PCI Optimization Recorded Case
Dr. Jonathan Hill:
Moving on from the acute coronary syndromes, this is a patient, 70 years old, who’s got a known history of significant coronary disease but with very significant co-morbidities: very severe aortic stenosis, with reduced left ventricular function, also has pulmonary sarcoidosis and Parkinson’s disease. She is highly symptomatic—multiple symptoms—really quite unwell: acutely dyspnoeic on a number of occasions, with paroxysmal nocturnal dyspnoea, orthopnoea, episodes of syncope and pre-syncope, and within the context of this acute hospital admission, presenting with symptoms of chest pain as well. Patient is being considered for trans-catheter valve implantation but also has significant coronary disease. What we’re going to be presenting here is the revascularization prior to this patient undergoing a trans-catheter valve procedure.
Revascularisation prior to TAVI:
How an angio co-registered OCT provides guidance for treatment
By Dr. Jonathan M Hill | King's College Hospital, UK
Dr. Jonathan Hill:
What we’re seeing here with these setup shots—I’m getting prepared to treat the lesion within the AV circumflex and the marginal. We’ve carried out OCT study, and this just going through the procedure of co-registration. It’s a fairly simple procedure. Just clicking on the vessel from distal to proximal, you can see the markers coming up there. Okay. This is making an assessment. This is a bifurcation lesion. We’re looking at the daughter vessel going into the mother vessel there. And you can see on this longitudinal views, with the angio co-registered pictures, that there is a very significant lesion. Of course, you could see that angiographically, but what we’re trying to do here and trying to achieve in these picture is make very precise measurements at…
Okay. This lady has aortic valve disease and is being prepared for a possible trans-catheter valve procedure. She has also got significant coronary disease and has had episodes of pulmonary edema. She’s got a dominant circumflex system and on previous angiographies, has been found to have significant disease in the dominant circ. You can see within this AV circumflex and large obtuse marginal. And there is also a potentially significant lesion in the left anterior descending artery.
We’re now assessing the circumflex. We’ve carried out balloon dilatation of very tight segment. This is supplying the inferior part of her heart and the lateral wall. You can see on the upper image, that was probably the area where we would land the distal stent, so I’ll put that as my distal marker. And we probably need to come up to here—just this segment here which is where that side branch is—and land the stent there. I’ll make that my proximal marker. I’ve chose that on the basis of the OCT image there. That’s the landing zone. This is the tight segment which we’ve just ballooned. You can see that very tight area here on the angiogram corresponding to this tight area on the axial view, and corresponding to this point here which is recorded as 1mm2, which is really a very tight lumen within this tight segment of this AV circumflex. We’re going to go here. I’m going to just adjust the position using the coronary angiogram. I want to drop my stent there. That’s where I would be on the OCT, and I’d make that my proximal marker. So there’s my read-out of the stent. I need something which is at least 2.8mm distally and slightly smaller because I’m going to flare it out. It’s going to be coming out here, make it right at the ostium. Re-do my proximal marker, so 2.5mm there. I think a stent in this segment is going to be at least a 2.5mm. I’m probably going to have to post-dilate it a little bit up to 2.75mm. I’d like a 2.5mmx24mm. I’m going to have a Synergy please.
We’re going to look again at the other branch. We’ll look again at this bifurcation, but his time going down the marginal rather than the AV circ. We’re definitely beyond that lesion. Proximal end is back in the guide. That’s got the marginal vessel. It’s got the bifurcation to the proximal AV circumflex. In fact, you’ll see from the anatomy here the almost separate origins of the left main. It’s not a particularly good quality study but I think it will be sufficient quality to be diagnostic just in terms of the estimate of the vessel size. Okay. Let’s accept that. We have got quite the size distally. I’ll come up here. This is where we think the bifurcation is. This is that tight segment. We’re then coming in to that bifurcation. Coming up here, you can see on the angiogram, we’re getting into the bifurcation now. In fact, this is the point here. This is really helpful because what you can see now is the lumen of the other vessel, and clearly a large-size lumen. And there’s the wire in the lumen of the other vessel. A bit proximal, now this is getting into the main lumen here. In fact, you can see it turning around the corner. It’s like a little car driving around the corner. There we are. That’s in the main lumen. This is the mother vessel, and this is large. And let’s see what sort of size this is. Now despite this being slightly suboptimal because of the clearance, we’re still able to make some accurate measurements here. I think I can turn on the measurements on the side. This is that proximal vessel, which if you’re estimating angiographically, you may say it’s a 3.5mm or a 4.0mm. That’s the mother vessel. And then each lumen down here distally... We don’t need to come back into that vessel because in fact… Let’s drive down to the origin. It’s quite tight there in the origin. We certainly need to treat the ostium of that vessel. And we need to work out our way. I’m going to T this. I’ll put a stent in here. And I’ll put my… Let’s just come down here. We’re treating here. Put on the lumen profile. You can see the step-up here in this calibre of the vessel, which is going from the daughter vessel into the main AV circumflex, which is at that point there. So I’m going to need a stent that will cover this segment here. I think probably we’ll read the size of that. That would be a 2mm—minimum of 2mm. Accept that calibration. And I think this is a question now of measuring the lumen rather than the vessel size. That would be what a 3mm stent in that segment would look like. Okay. Can I have 3mm balloon please? And a 2.75mmx20mm Synergy please? This is going down in the AV circ. We’re just going to position this across the origin of the… and pull the stent back on to it. Let’s park that down there. Can we have another second indeflator please? And have a stent as well? Now we’re going to position the stent in the marginal. Okay. Come to the PA caudal please.
This is the position here. If you look at the angio co-registered image, that’s origin, orifice, or ostium of the marginal, and that’s where we’re trying to position. On angiography, we’re hoping it’s in that position… which is where it is. I’m going to pull it back a little bit more. You’ve got the stent there. Okay. Up we go please. That’s back into the main vessel and down. Take the stent balloon out. Up again on the main vessel. Okay. Looks okay. A little bit of edge effect on the… Can we have a 2.75mmx8mm please? Let’s pull this back first. Let’s see. It may just be a conformability or bendability issue in the vessel.
Here, I want the lumen size at this point here. Actually, about there. And then proximally, I’m going to come up to about… and this is where I lose. The decision is whether we stent across or can we position exactly here? I think we can probably… Actually, you can see where the side branch is coming in. And there’s disease there, so in fact we have disease at both ostia. In fact, I’m going to bring it back into this vessel, and I’ll post-dilate it in this proximal segment here. We’ll use a 30mm stent—32mm. Let’s look at this segment here, how we’re going to size this. We can put the measurements on. You can see, this is the main luminal diameter. We’ll need at least that size in the stent. Let’s use EEM in this horizontal—that’s 3.5mm. I’m not sure if you needed OCT to tell if this was a 3.5mm vessel, but it certainly has helped in the degree of precision and the length especially in this fore-shortened area with this AV circumflex in the AV groove. So I’m going to put in a 3.5mmx32mm. I’m going to post-dilate the proximal segment with a 4mm balloon. Now it looks fine. Just bring up my pictures. Coming down, landing it down here… so that’s about a 32mm there in that position. Can you give us a little tester? Okay.
I’m going to… looking at the measurements, at 14 the external diameter of Synergy here is 3.86mm.
Co-registered image. I know where the proximal end of my stent is. I’ll drive the car out there. Let’s do that. Here we are up here. That’s it. The proximal end of my stent is there, and you can see the size of the vessel. Let’s have a measurement. And let’s look at the other dimension. Even though this wasn’t really a perfect picture, the diagnostic information is good. If I get a 4mm balloon, proximal optimization, so I need a short 4mm. 4mmx8mm, please. And that should be fine. Come back to the spider view please. Up we go please. We’re right at that bifurcation. We’ve got a few millimetres. Up we go. And down.
That looks better than before. And if our OCT measurements are right, then this should all be apposed. Let’s have a look. Okay bring this up please. Bring this up more. More. Keep coming. That’s it. Okay. I’ve just caught a flash of possibly an un-apposed edge there, but we’ll see it on the reconstructed view. Another point. Another point here. Point here. Oops. Point here. Let’s see. Seems good enough. Let’s go down to the end of the stent. Just here, well-apposed. Coming in let’s have a look. Yes, nicely apposed. You can see this getting into the area where there’s quite a lot of plaque. Possibly slightly under deployed here. We might actually just post-dilate that segment, but we’ll have a closer look with the lumen contour. Not that good clearance here. Remember this was the extremely tight segment, which we had to pre-dilate to even get the OCT catheter down. Now we’re coming to the bifurcation. You can see on the angio picture, that’s where we are. Just here. And we should be able to see, if I can rotate around. Yes, there you can see. That’s the point. We’ve got the stent struts over the origin of the marginal. This is a large-cell stent, so I’m not going to open this up. And let’s come back to the proximal segment. I’ll drive the little car up here. And this is where I’m hoping we’ve got good apposition. This is the edge. Coming in to the edge of the stent, you can see that here. That’s the stent struts here are well apposed. That’s post-dilatation in the mother vessel with a 4mm, and it all looks fine. Can I have a 3.5mmx20mm non-compliant? We’ll just do that segment further down.
The segment we’re going to post-dilate is this one here. Coming down, let’s see if we can do a lumen profile. We should get some idea from the lumen profile of under expanded areas. It’s pretty good. This is the view here of the stent in 3 dimensions. This is the appearance. And we can rotate. Now we can see a well-apposed stent. You can see this is where the other stent is coming in. You can get an idea of the post-dilation here of the proximal mother vessel and the daughter vessel here. If we rotate around again, this is a very nice view showing us the stent strut architecture and the apposition within this vessel. Let’s take some final shots. Looking good. Come to the RAO caudal. And PA caudal. Okay.
Discussion
Dr. Jonathan Byrne:
Thank you Jonathan for another elegant demonstration and a complex case—elderly patient, coronary disease, significant aortic stenosis, poor left ventricular function. Very nice demonstration of anatomy and coronary intervention bifurcation. Perhaps I could ask Narbeh, why not FFR here?
Dr. Narbeh Melikian:
It’s a very good question. FFR is a very useful index, but there are physiological limitations to when it may not provide the most accurate information. In this case, there are a number of issues. First, the patient has significant aortic stenosis, a bicuspid aortic valve. There is some element of left ventricular damage (fibrosis), an element of left ventricular hypertrophy, on a background of an impaired ventricle. Each one of those various factors can in isolation give us a false FFR reading. When you combine them all together, it would probably be an uncharted use of FFR to determine the physiological significance of a vessel. The other thing that I would potentially be slightly uncomfortable with is administration of intravenous adenosine to someone who has critical aortic stenosis. In case that were to cause significant haemodynamic problems or complete heart block, I’m not sure how well the patient’s heart would tolerate all of them. All in all, I don’t think this is a good case for FFR. And this is one example of where intravascular imaging would be not only safer, but it may also provide the information that you need as we have seen in the case.
Dr. Jonathan Byrne:
Thank you. Turning to the procedure itself, Jonathan, if we look at the use of OCT, it gives us intensely detailed information about plaque composition and structure over and above that given by intravascular ultrasound. Would you agree or disagree?
Dr. Jonathan Hill:
Well, this is a case that could have been done with IVUS, but if you have a modality available where the spatial resolution and the accuracy is higher, well, why not use it? I think in this particular case, the precision for treatment of this bifurcation, the OCT really gave you that almost micron scale resolution which you just can’t get with IVUS. Absolutely, it’s possible to do it with IVUS, but I think the key for this case, for getting the stent size is right, was being able to assess the vessel size, so looking at EEM measurements. And we can do that easily with OCT. I think one of the criticisms that people who are proponents of IVUS have is that OCT doesn’t allow you to see the tri-laminar structure of the vessel. But I think all of the images we’ve got here, the vast majority of the sections that we can see, we can see the full vessel structure. And then when you’re taking pictures to guide stent placement, if you want that millimetre micron scale precision, you don’t really get that with IVUS. I think the accuracy of being able to contour the lumen, measuring the precise lengths, precise diameters, you really get with OCT. Here, the decision was made to proceed with intervention prior to the case going on the table. We’re going to treat the AV circumflex, the marginal, and the LAD, which is what we did. This was really where OCT and the co-registration came into its own where we matched up the exact vessel-size, the exact position on the angiogram. It guided us exactly where we’re going to put the stents. It helped guide us to make the decision about how we were going to approach this bifurcation. Was the disease exactly at the ostium? What technique were we going to use for this bifurcation? I didn’t really want to use a Culotte technique or Crush technique because of the mismatch in the mother vessel size with the marginal. This particular technique, making the measurements, was ideally suited to using OCT.
Dr. Jonathan Byrne:
And you nicely covered the ostium of the marginal. Some are slightly back into the main vessel. It looked beautiful. I think the size as a match was a big issue in deciding on the bifurcation situation here. And I think even without OCT, you can decided on that. But OCT gave us such nice additional information about the anatomy.
Dr. Jonathan Hill:
One thing I think OCT teaches you in treatment of bifurcations is that up until relatively recently, you know the Mantra wars, final kissing balloon inflation. Now, the problem with final kissing balloon inflation is when you’ve got a round stent in the proximal vessel (in the mother vessel), and you have two round structures inside, it distorts the architecture of that stent, maybe only slightly changing it from a round architecture to a slightly ovoid architecture. And in that process, you can see with OCT where the stents struts are then lifted off at the carina. I think that really OCT provides justification for proximal optimization. We’ve dealt with each limb here, but the final inflation here is proximal optimization, avoiding going down either limb.
Dr. Jonathan Byrne:
And perhaps another thing to mention in that setting which is often forgotten is the use semi-compliant rather than non-compliant balloons because you often find with OCT that a non-compliant—because it’s a fixed and rigid volume—it does not necessarily appose the struts. I think it is a very useful information and teaches them more how to stent.
Dr. Jonathan Hill:
Absolutely.
Dr. Jonathan Byrne:
Thank you.
Is Angio Enough to Make a Good Decision in ACS?
Dr. Jonathan M Hill | King's College Hospital, UK
Dr. Jonathan Hill:
Welcome! My name is Jonathan Hill. I’m a consultant cardiologist. I’m speaking here from King’s College Hospital, which is a large cardiac centre in South London. We’re going to be talking today about the growing role of OCT in acute coronary syndromes.
Many of us are familiar now with the technology of OCT, and, I think, our familiarizing ourselves with the way in which OCT integrates within our clinical practice. We’ve been using it as an everyday tool here at King’s. And there are many stages of patients’ journey through the cath lab where I think OCT has a use. I think when we’re talking about the indication today, I think there are many aspects of OCT which lend itself very well to the use within acute coronary syndromes.
Let’s think about the very stages of intervention that patients go through. In the pre-interventional stage, OCT has many roles: identifying plaque characteristics, looking at lesions for diagnostic purposes, and I think that’s of a special use now, looking at plaque characteristics in acute coronary syndromes—looking for plaque rupture. And then when you come to the interventional procedure itself, the practical aspects of OCT that its everyday integration into our workflow is that we can size stents very accurately. We can gather a clear decision made about stent length and stent diameter. We can choose our balloons. And following stent deployment, we can immediately check stent apposition. We’re all familiar with these capabilities. And there’s also a role in the post-interventional phase, which is looking at strut coverage and stent thrombosis.
Pre-Intervention
Let’s just focus on the pre-interventional stage, and let’s just remind ourselves that the clear advantage of OCT is spatial resolution. This is a picture many of you will have seen presented previously which clearly shows us that the three-layered vessel can be clearly seen with OCT. We can see the intimal layer. We can see the media. And we can see the adventitial layer. The identification of normal vessel, I think, can be done better with OCT than other intravascular imaging modalities. And you apply that principle of high endoluminal definition in multiple different plaque scenarios. You can see here going from the calcified plaque, a fibroatheromatous plaque, lipid-rich plaques, plaques which may have ruptured associated with thrombus, and calcification and thrombus at the same time. All of these levels of detail, you can see with a much higher spatial resolution than you can with intravascular ultrasound.
This is a typical 40 mega-hertz picture from IVUS looking at a dissection or a vessel that is suspected of having dissected. I think it’s quite difficult to interpret this IVUS pictures if you’re not used to looking at them. You need quite a lot of training in the interpretation. Now that training in interpretation isn’t required to the same degree with OCT. Clearly, we see the dissection plaque here indicated in this right panel. We can see the plaque. We can see the stent struts. And this is a very clear demonstration of a significant advantage in spatial resolution of OCT compared to IVUS.
This clearly shows that tri-laminar structure. The three-layered vessel wall has been disrupted, and what we see is a dissection and a false lumen. In fact, this is a fairly well-known picture that goes around in various presentations for this is showing the imaging within the false lumen in a dissection plaque.
Interventional Guidance
Let’s think about interventional guidance and, in particular, looking at patients who present with ischaemia perhaps in the context of an acute coronary syndrome.
Angio and OCT to guide everyday intervention
This is a patient who presents with symptoms typical of ischaemia, who happens to come to the cath lab, has previously had a non-invasive myocardial perfusion test done. You can on the panel here on the left, there is a lesion within the proximal AV circumflex. You can see the tortuosity within the left anterior descending artery, but there isn’t really any focal lesion in the same way that there is within the circumflex that stands out from this particular projection. Well, let’s look at the OCT. This is the OCT taken in the circumflex artery, and this really just shows the high-resolution imaging. We’re getting all the images here. We can clearly see there’s a lesion here. We can move backward and forward through the lesion. We can see a fairly significant coming out nearly down to or under 2mm2. From an OCT perspective, and angiographically, this looks significant. You therefore proceed, as you would normally, to intervention of this vessel. And this is this vessel now, successfully stented.
That would seem a straightforward use of OCT to guide intervention in a patient with ischaemia.
However, in this particular patient, the ischaemia is antero-apical. The non-invasive test, we didn’t carry out a pressure wire study in this particular case, but the ischaemia is clearly antero-apical. Let’s have a look, because we’re looking at the left anterior descending artery in a different projection. What we can see here is perhaps there is an area within the LAD we may be suspicious. Let’s look with the OCT. We’re looking distally. We can see the lumen size there—2.8mm to 2mm2—coming through the lesion. In fact, we see a very tight focal stenosis—1.4mm2. In fact, by OCT measurements using this cross-sectional lumen, there clearly is a significant lesion in the left anterior descending artery. In fact, this is a lesion which would clearly be sufficient to generate myocardial ischaemia, and has been demonstrated to do so on a myocardial perfusion study. The patient is then treated using OCT to guide the process, and in fact, this patient was then subsequently treated with stent implantation in the usual fashion under OCT guidance. So this is a situation where OCT will help with diagnosis. It would help with lesion assessment. Here, it actually made the diagnosis, guided the intervention, and the final result (the stent apposition) was also then confirmed with OCT. So OCT here was instrumental in diagnosis and in treatment of the lesion.
ACS Diagnosis
Angio with OCT Guidance
This is a patient that we see presenting very frequently in acute coronary syndrome. And in this patient, you can see in these various projections of the LAD, there is a plaque within the proximal segment of the left anterior descending artery. Now, this is an important lesion to treat. It’s in a prognostically significant position. We’ve got a distal lesion within the LAD. Of course, we can address this as well. And we can see in this PA caudal projection, in this segment here—I hope that you can see this on your computers at home—that there is a section within this vessel where it appears hazy, but the limits of spatial resolution of the coronary angiogram do not enable us to make a precise pathological diagnosis. This is a lesion that we would look at, and the experienced interventionist will say, “Well, yes, it looks a bit hazy. Certainly, you’re going to intervene in this region.” But we then carry out OCT, and in fact, here at the ostium of the left anterior descending artery is the plaque rupture. This is the confirmation that this patient has presented with a plaque rupture event. This patient transiently may have had vessel occlusion. Once the plaque had ruptured, the thrombus is now gone (the thrombus that had formed), but this is an acute coronary syndrome presentation. OCT has clearly shown plaque rupture. Now once you’ve got that information, it confirms you diagnosis. And it confirms the diagnosis with a level certainty that you could not achieve with intravascular ultrasound.
OCT to guide ACS Treatment
In this particular case, once we go that information, diagnosis had been made, we then treated the distal lesion. In this case, we used bioresorbable scaffold, and we then treated the proximal lesion within the left anterior descending artery here with two further scaffolds. And once that’s done, we’ve used that to guide the scaffold size. OCT particularly lends itself to the technology of bioresorbable scaffolds. We can see in fact an interesting phenomenon that you see on a scaffold on OCT. It’s fairly round at the end of the lesion in the proximal segment of the LAD, and then going into a more oval shape, with well-preserved overall MLA. This shows the conformability of the scaffolds within this vessel. And in fact, we can confirm that we’ve got exact positioning at the ostium of the left anterior descending artery with very precise positioning of the scaffold within the LAD. All of this is done with OCT guidance.
IVUS vs OCT
When you compare the use of OCT to make these precise measurements, really there isn’t any other modality that will compare with it. IVUS gives you some information, but when we’re looking at the deployment of stents… And it’s especially important when you’ve got these scaffolds that they are properly deployed because they got quite thick struts. And also in the context of precise positioning at the ostium of a vessel like the LAD, I want to know whether the stent that I have deployed, the scaffold I have deployed, is exactly sized to the vessel.
Now, perhaps with a lot of training, you can appreciate that there is a degree of mal-apposition of this stent using the IVUS. But in fact, really when you’ve got a modality available like OCT, why use anything else when you’ve got such a precision, and the measurements you can make with such a high degree of accuracy. To my mind and to my eye, OCT in this context for guiding stent deployment and apposition is really the number one modality. These are the same sections of the artery looked at with a 40 mega-Hertz intravascular ultrasound, and this is the same image taken using OCT.
Multi-vessel Intervention
We’ve been using OCT to guide patients having a more complex intervention for multi-vessel disease. This is not a particularly complex set of lesions, but this is a patient who was referred for coronary artery bypass surgery, had widespread ischaemia, having presented in the context of an acute coronary syndrome. What we can see here is this left-sided system with these two marginal, and in the LAD there is a significant lesion. The patient is turned down for surgery because of co-morbidities. And then is referred back to us as the interventionist, and so we’re asked to then intervene. We used OCT in this particular scenario for vessel sizing for every vessel. And this was used because we were deploying bioresorbable scaffolds. In fact, we’re taking pictures here of every single vessel. We apply this principle. Maybe we need to do a bit of pre-dilatation with a balloon. You can see some of the prep work done to this vessel. We’re using fairly large-sized balloons, at least a 1:1 balloon to vessel ratio, which is the method that we have adopted for bioresorbable scaffold implantation to get the sizing precise. And then we can use all the measurements that we have taken to precisely size the scaffold and get the positioning exactly right. And so we go in the end from fairly significant multi-vessel disease to a very satisfactory angiographic result, and also a very satisfactory OCT-guided result. And this patient has been completely revascularized. All done under OCT guidance.
Overlapping Bioresorbable Scaffolds
This is the type of view you will get, and in fact you can appreciate with this spatial resolution—you can’t see this on IVUS—with the bioresorbable scaffolds, struts standing on top of one another.
Post Intervention
There is also an application for OCT in the post-interventional phase, often in acute coronary syndrome. This is a patient presenting with a thrombus within that stent. OCT helps at looking at the reason for stent failure, whether it’s caused by neo-intimal proliferation, whether it’s neo-atherosclerosis, or whether it’s a stent thrombosis on top of neo-intimal proliferation, as in this case.
Same Vessel: IVUS or OCT?
This is a patient for follow-up who… we’re looking at this patient three years after bioresorbable scaffold implantation. And what we can see is the same section of artery being imaged. Have a look at the IVUS picture here. Can you actually see the scaffold here? I think it’s quite hard to actually discern exactly where the scaffold is in this vessel. Perhaps with a lot of training, you can work out where it is. But I think when you come to the high resolution imaging, what we can clearly see here, and you can see coming in to the axial views now, you can see the stent, the scaffold struts within the wall of the artery. This stage, this is over two years after implantation. These are the spaces where the struts would have been, but they have now almost completed their process of bioresorption.
OCT Follow Up after CTO
We’re also using OCT in other applications for follow up. This is an example of OCT follow-up after chronic total occlusion. This is an example of a patient with a long segment of disease in the left anterior descending artery who’s undergone antegrade dissection/re-entry using the Bridgepoint and CrossBoss and Stingray procedure. In these particular cases, we’re interested at looking at vessel healing. And I think OCT is the modality to do that. What we see is that there looks to be an angiographically well-healed vessel. We then come to the OCT pictures. We’re looking at fairly good healing here—neo-intimal coverage. And what we see within this area is probably the dissection and re-entry zone. This really shows the capabilities of OCT to track vessel healing even late after stent implantation.
Angio and OCT Co-registration
OCT, I think, is just one piece of the picture now in the management of acute coronary syndromes. Where I think the power of OCT is going to be increased even further is where we can directly cross-reference OCT with angiography. We’re going to be looking at some case examples. This is one of the first cases in St. Jude which demonstrates the theoretical possibility of co-registering this image here, or your longitudinal image, with your angiogram. This actually increases the level of precision even more. When we’re looking at OCT for stent guidance, for making the diagnosis, looking for plaque rupture, we can find out exactly where on the angiogram the OCT is showing pathology.
Automated Strut Detection / Coverage
There’s also more software in the pipeline coming from St. Jude with automatic strut detection. Here we see the stent struts lit up as red, and these are the mal-apposed struts we can see within this cross-sectional image. This technology is coming to an OCT machine near you very soon.
The Growing Role of OCT in ACS
To summarize, there certainly is a growing role of OCT in acute coronary syndromes. It’s useful in the pre-interventional phase as a diagnostic aid. It’s very useful for guiding interventions both simple and complex in ACS patients and stable patients. It’s useful in single and multi-vessel disease. And it’s also a useful tool to follow-up stent performance.
Thank you very much.
Discussion
Dr. Jonathan Byrne:
Thank you Jonathan for another elegant talk. I think the cases today and the discussion around the use of physiology with fractional flow reserve and anatomy with OCT demonstrate that whilst we think that we’re pretty good as interventional cardiologists looking at the coronary angiogram, in most or many of the interventions we carry out today, it’s simply not enough. We need that additional information. We certainly need physiology to guide when we should place stents, and the anatomy gives us the detailed information as to how we should place and how they perform after the procedure has been done. One might think that having looked at all this information, we should be using this in every case. But that’s simply not practical. Perhaps I would like to ask Jonathan where he thinks the limitations of this new technology lie, and how we might overcome that.
Dr. Jonathan Hill:
Well, I think you’re right that it probably isn’t practical to use it in every case: in a Type A lesion, you’ve clearly made a judgment about vessel size; the cath lab is a busy place; there’s new cases waiting; the troop or the workflow has to be maintained. If you’re using OCT very infrequently, perhaps there’s an incentive not to use it because it delays things. If you use it all the time, then the cath lab becomes very slick. I think we are a fairly regular user of OCT here, and I don’t think it really significantly disrupts the workflow. I think people are concerned about slowing cases down over complicating cases. There’s even been a concern that you’re getting too much information—an information that you don’t know what to do with. I don’t really understand that argument of having too much information. I think the argument really is what you do with the information once you have it, and I think we’re still in that evaluation phase. But I think, as we are biologists and scientists as well as physicians, one of the things that I think OCT gives us is it’s actually teaching us about the pathology of atherosclerosis. It’s teaching us about the way in which we have to treat plaque. And especially I think in some of the cases we have shown with acute coronary syndromes, the questions we’re asking are—you know, when you see plaque rupture, I think this is a very important academic question that Narbeh touched on earlier—if we see plaque rupture, a process of pathology that’s unfolding in front of you, how should that piece of information influence our decision making? A large number of our patients have acute coronary syndromes. It’s a large proportion of the workload of any cath lab. I think in terms of its limitations, well, I don’t see any limitation that’s going to reduce its use. I think its limitations are is that it’s giving you such good information that you want to use it in every case. I mean, not quite every case but almost every case.
Dr. Jonathan Byrne:
Thank you. One comment I might make is that this is a case certainly of the anatomy and the imaging racing ahead of the scientific literature. And we all think we know what we should do with a plaque rupture, and it has to be said that we are still waiting for the evidence-based to support a lot of the way treat acute coronary plaque rupture, but I think it will catch up. We will get there. And this is a certain case where the imaging gives us information first.
Dr. Jonathan Hill:
There are so many trials now in process around the world—in Europe. Some of these trials are sponsored by St. Jude; some of them are academically led studies. All of these questions are being asked right now. And I think we are going to see over the course of the next few years some really interesting clinical data emerging involving the use of OCT in multiple different settings, whether it’s acute coronary syndromes, bifurcations, stent follow up, looking at strut coverage. It’s now the default tool for looking at stent performance in a research setting. All the device companies are interested in using OCT to assess their stent performance. I think that data is being gathered now. I don’t think we’re proceeding with the expansion of OCT without a very strong parallel process going on of research into its effects on outcome. And I think that’s the key piece of information that we need which we’re currently lacking. That is the current limitation: is there any effect of OCT on clinical outcome in the long-term? I think that question has to be answered.
Dr. Jonathan Byrne:
Perhaps I could turn to Narbeh very briefly. FFR, a mature technology, has been with us for 20 years or more. If you look at the experimental studies, it gives us the answer we need on many occasions in the cath lab. Are there any important unanswered questions it needs to tell us? Or do we have all the information we need?
Dr. Narbeh Melikian:
There are always unanswered questions. But I think at this stage in the natural history of the technology, I think what is more important, in my view, is that your limitations to use of FFR—I’ve alluded to some of them—although, it remains certainly, in my view, the most important physiological index that we could use. What I think the future will bring, in my view, if I could look in a crystal ball, is that we will combine the physiology with the anatomy at the same time. And this is extremely important because we’re talking about individualized treatment of cases at every level in medicine. This is certainly coming in my view to the cath lab where we will be able to use perhaps novel technologies combining the physiological index that we get with the anatomy. And the anatomy would be used at the end of the procedure. And we start the procedure with the physiology.
And following of the comment that Jonathan has made a few moments ago, where is the limit? Should we be using, for example, OCT in every one? History tells us that technology is developed. And the field of interventional cardiology in particular has seen very, very major advances extremely quickly. We’ve moved from simple balloon angioplasty to bare metal stents. We’ve moved from bare metal stents to everyone getting a drug-eluting stent very rapidly. We use OCT now fairly sparingly. And with improvements in technology which would make the whole thing much more rapid, I can envision the time will come that if with the data supports that, for example, that stent apposition in a certain pattern gives us a better outcome, that every stent will get an OCT. And with that potentially will come novel technologies which will allow us to do that much, much more rapidly—guide wires which would allow us to acquire sort of OCT at the same time. Who knows what the future will bring?
Dr. Jonathan Byrne:
I think that’s a very eloquent way to end this discussion. The use of established and new technologies and combining them into a single approach to coronary artery is a very important paradigm we should strive for. And it may not be with us now, but it may be common place in 5 or 10 years. I think this session today has shown us the utility of FFR, the utility of OCT, both in pre-lesion assessment and post-stent deployment. I think it is going to grow in a very sure fashion across within the UK, Europe, and the world. And I’d like to end now. I’d like to thank my fellow participants. Thanks St. Jude. And I also would like to say that the cases recorded today will be available in the web later this evening. And in addition, there’s one further case that was recorded which we didn’t have time to show. All of it will be available. And I’m sure that your comments and questions will still be welcomed and answered late until the evening. Thank you very much.
Participer à la discussion
Suggestions
San Francisco : Jeudi 27 mars 2025 de 22h à 12h (GMT+1)
New York : Vendredi 28 mars 2025 de 01h à 15h (GMT+1)
Buenos Aires : Vendredi 28 mars 2025 de 03h à 17h (GMT+1)
London / Dublin : Vendredi 28 mars 2025 de 06h à 20h (GMT+1)
Paris / Berlin : Vendredi 28 mars 2025 de 07h à 21h (GMT+1)
Istanbul : Vendredi 28 mars 2025 de 08h à 22h (GMT+1)
Moscou / Dubaï : Vendredi 28 mars 2025 de 10h à 00h (GMT+1)
Bangkok : Vendredi 28 mars 2025 de 13h à 03h (GMT+1)
Shanghai : Vendredi 28 mars 2025 de 14h à 04h (GMT+1)
Tokyo : Vendredi 28 mars 2025 de 15h à 05h (GMT+1)
Sydney : Vendredi 28 mars 2025 de 16h à 06h (GMT+1)
Wellington : Vendredi 28 mars 2025 de 18h à 08h (GMT+1)
Complex & High-Risk Indicated Procedures
Discover the 6th edition - Day #1
San Francisco : Lundi 10 juin 2024 de 08h à 09h (GMT+2)
New York : Lundi 10 juin 2024 de 11h à 12h (GMT+2)
Buenos Aires : Lundi 10 juin 2024 de 12h à 13h (GMT+2)
Reykjavik : Lundi 10 juin 2024 de 15h à 16h (GMT+2)
London / Dublin : Lundi 10 juin 2024 de 16h à 17h (GMT+2)
Paris / Berlin : Lundi 10 juin 2024 de 17h à 18h (GMT+2)
Istanbul : Lundi 10 juin 2024 de 18h à 19h (GMT+2)
Moscou / Dubaï : Lundi 10 juin 2024 de 19h à 20h (GMT+2)
Bangkok : Lundi 10 juin 2024 de 22h à 23h (GMT+2)
Shanghai : Lundi 10 juin 2024 de 23h à 00h (GMT+2)
Tokyo : Mardi 11 juin 2024 de 00h à 01h (GMT+2)
Sydney : Mardi 11 juin 2024 de 02h à 03h (GMT+2)
Wellington : Mardi 11 juin 2024 de 04h à 05h (GMT+2)
L’OCT dans la resténose et thrombose de stent – il est temps d’allumer la lumière !
L’imagerie : un outil indispensable pour gérer les complications post-angioplastie
San Francisco : Mercredi 4 octobre 2023 de 09h à 09h45 (GMT+2)
New York : Mercredi 4 octobre 2023 de 12h à 12h45 (GMT+2)
Buenos Aires : Mercredi 4 octobre 2023 de 13h à 13h45 (GMT+2)
Reykjavik : Mercredi 4 octobre 2023 de 16h à 16h45 (GMT+2)
London / Dublin : Mercredi 4 octobre 2023 de 17h à 17h45 (GMT+2)
Paris / Berlin : Mercredi 4 octobre 2023 de 18h à 18h45 (GMT+2)
Istanbul : Mercredi 4 octobre 2023 de 19h à 19h45 (GMT+2)
Moscou / Dubaï : Mercredi 4 octobre 2023 de 20h à 20h45 (GMT+2)
Bangkok : Mercredi 4 octobre 2023 de 23h à 23h45 (GMT+2)
Shanghai : Jeudi 5 octobre 2023 de 00h à 00h45 (GMT+2)
Tokyo : Jeudi 5 octobre 2023 de 01h à 01h45 (GMT+2)
Sydney : Jeudi 5 octobre 2023 de 03h à 03h45 (GMT+2)
Wellington : Jeudi 5 octobre 2023 de 05h à 05h45 (GMT+2)
Guides de 1ère intention :
algorithme décisionnel de la lésion simple à la lésion complexe
San Francisco : Vendredi 28 mars 2025 de 22h à 12h (GMT+1)
New York : Samedi 29 mars 2025 de 01h à 15h (GMT+1)
Buenos Aires : Samedi 29 mars 2025 de 03h à 17h (GMT+1)
London / Dublin : Samedi 29 mars 2025 de 06h à 20h (GMT+1)
Paris / Berlin : Samedi 29 mars 2025 de 07h à 21h (GMT+1)
Istanbul : Samedi 29 mars 2025 de 08h à 22h (GMT+1)
Moscou / Dubaï : Samedi 29 mars 2025 de 10h à 00h (GMT+1)
Bangkok : Samedi 29 mars 2025 de 13h à 03h (GMT+1)
Shanghai : Samedi 29 mars 2025 de 14h à 04h (GMT+1)
Tokyo : Samedi 29 mars 2025 de 15h à 05h (GMT+1)
Sydney : Samedi 29 mars 2025 de 16h à 06h (GMT+1)
Wellington : Samedi 29 mars 2025 de 18h à 08h (GMT+1)
Complex & High-Risk Indicated Procedures
Discover the 6th edition - Day #2
San Francisco : Mercredi 23 novembre 2022 de 07h à 08h (GMT+1)
New York : Mercredi 23 novembre 2022 de 10h à 11h (GMT+1)
Buenos Aires : Mercredi 23 novembre 2022 de 12h à 13h (GMT+1)
London / Dublin : Mercredi 23 novembre 2022 de 15h à 16h (GMT+1)
Paris / Berlin : Mercredi 23 novembre 2022 de 16h à 17h (GMT+1)
Istanbul : Mercredi 23 novembre 2022 de 17h à 18h (GMT+1)
Moscou / Dubaï : Mercredi 23 novembre 2022 de 19h à 20h (GMT+1)
Bangkok : Mercredi 23 novembre 2022 de 22h à 23h (GMT+1)
Shanghai : Mercredi 23 novembre 2022 de 23h à 00h (GMT+1)
Tokyo : Jeudi 24 novembre 2022 de 00h à 01h (GMT+1)
Sydney : Jeudi 24 novembre 2022 de 01h à 02h (GMT+1)
Wellington : Jeudi 24 novembre 2022 de 03h à 04h (GMT+1)
UNCAGE coronaries - Episode 3 : UNCAGE chronic total occlusions
San Francisco : Vendredi 20 octobre 2023 de 08h à 10h15 (GMT+2)
New York : Vendredi 20 octobre 2023 de 11h à 13h15 (GMT+2)
Buenos Aires : Vendredi 20 octobre 2023 de 12h à 14h15 (GMT+2)
Reykjavik : Vendredi 20 octobre 2023 de 15h à 17h15 (GMT+2)
London / Dublin : Vendredi 20 octobre 2023 de 16h à 18h15 (GMT+2)
Paris / Berlin : Vendredi 20 octobre 2023 de 17h à 19h15 (GMT+2)
Istanbul : Vendredi 20 octobre 2023 de 18h à 20h15 (GMT+2)
Moscou / Dubaï : Vendredi 20 octobre 2023 de 19h à 21h15 (GMT+2)
Bangkok : Vendredi 20 octobre 2023 de 22h à 00h15 (GMT+2)
Shanghai : Vendredi 20 octobre 2023 de 23h à 01h15 (GMT+2)
Tokyo : Samedi 21 octobre 2023 de 00h à 02h15 (GMT+2)
Sydney : Samedi 21 octobre 2023 de 02h à 04h15 (GMT+2)
Wellington : Samedi 21 octobre 2023 de 04h à 06h15 (GMT+2)
Bifurcation PCI: an immersive experience
Live cases from the Visible Heart® Lab
San Francisco : Vendredi 10 novembre 2023 de 16h30 à 19h (GMT+1)
New York : Vendredi 10 novembre 2023 de 19h30 à 22h (GMT+1)
Buenos Aires : Vendredi 10 novembre 2023 de 21h30 à 00h (GMT+1)
London / Dublin : Samedi 11 novembre 2023 de 00h30 à 03h (GMT+1)
Paris / Berlin : Samedi 11 novembre 2023 de 01h30 à 04h (GMT+1)
Istanbul : Samedi 11 novembre 2023 de 02h30 à 05h (GMT+1)
Moscou / Dubaï : Samedi 11 novembre 2023 de 04h30 à 07h (GMT+1)
Bangkok : Samedi 11 novembre 2023 de 07h30 à 10h (GMT+1)
Shanghai : Samedi 11 novembre 2023 de 08h30 à 11h (GMT+1)
Tokyo : Samedi 11 novembre 2023 de 09h30 à 12h (GMT+1)
Sydney : Samedi 11 novembre 2023 de 10h30 à 13h (GMT+1)
Wellington : Samedi 11 novembre 2023 de 12h30 à 15h (GMT+1)






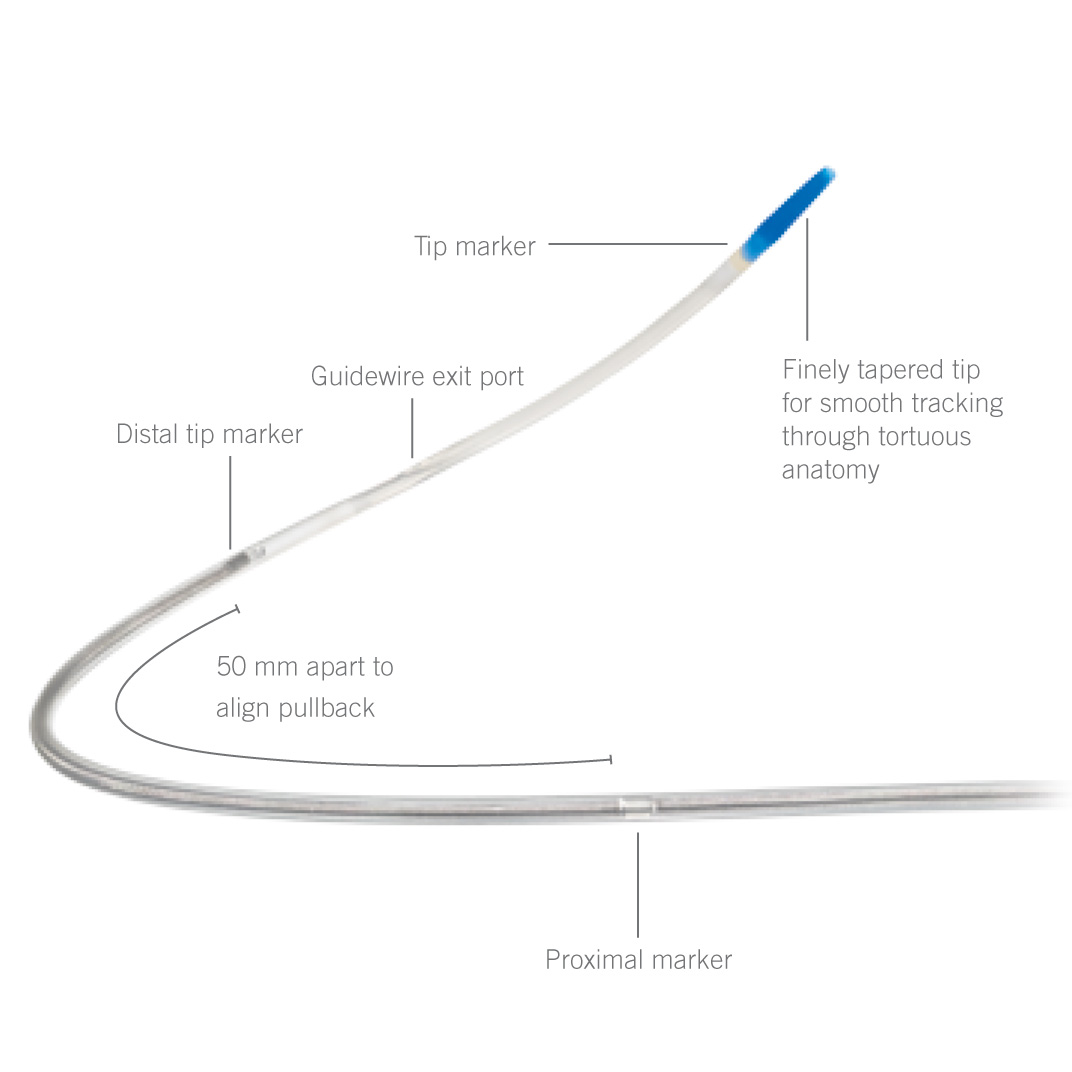



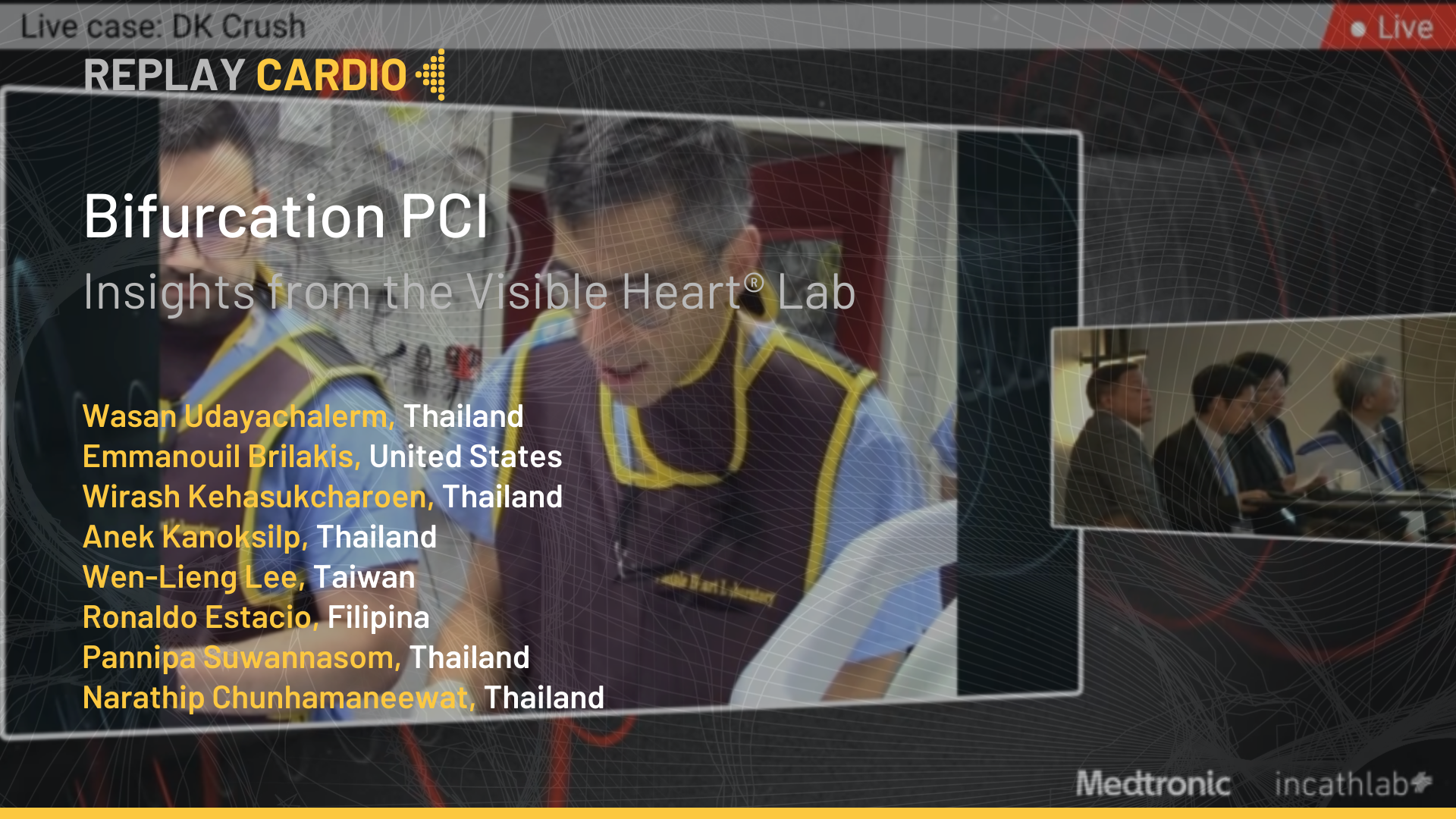

Alcides Z. In the case of bifurcation I think that is need to perform kissing-bolloon in the end of the procedure.Please comment that
maher T. good job